See Prompt in action!
Burnout is an epidemic amongst clinicians, and while there are several contributing factors, documentation burden is not only one of the most significant culprits, it’s also an unnecessary one.
Prompt asked 215 rehab therapists who are members of The Clinician Transition, an online community for rehab therapists (PTs, OTs, and SLPs) who are either considering a nontraditional role or have already taken one, why they are considering leaving traditional patient care.
79% of respondents under age 30 reported excessive workload as their reason for leaving, and 68% of total respondents said emotional burnout was a top reason.
AI solutions have entered the healthcare scene and are here to stay. They offer clinicians a way to document better, code more accurately, and help improve organizational outcomes while reclaiming the other parts of their lives that bring them joy and fulfillment.
This means engaging with family at home without the distraction or pressure of catching up on notes. It's also the time and energy to pursue hobbies and goals outside clinic hours without the weight of long sign-off times and open charts looming.
%2520(5).png)
While documentation styles aren't one-size-fits-all, there are some common behavior patterns in how rehab therapists approach their documentation to complete their notes along with the rest of the clinic responsibilities.
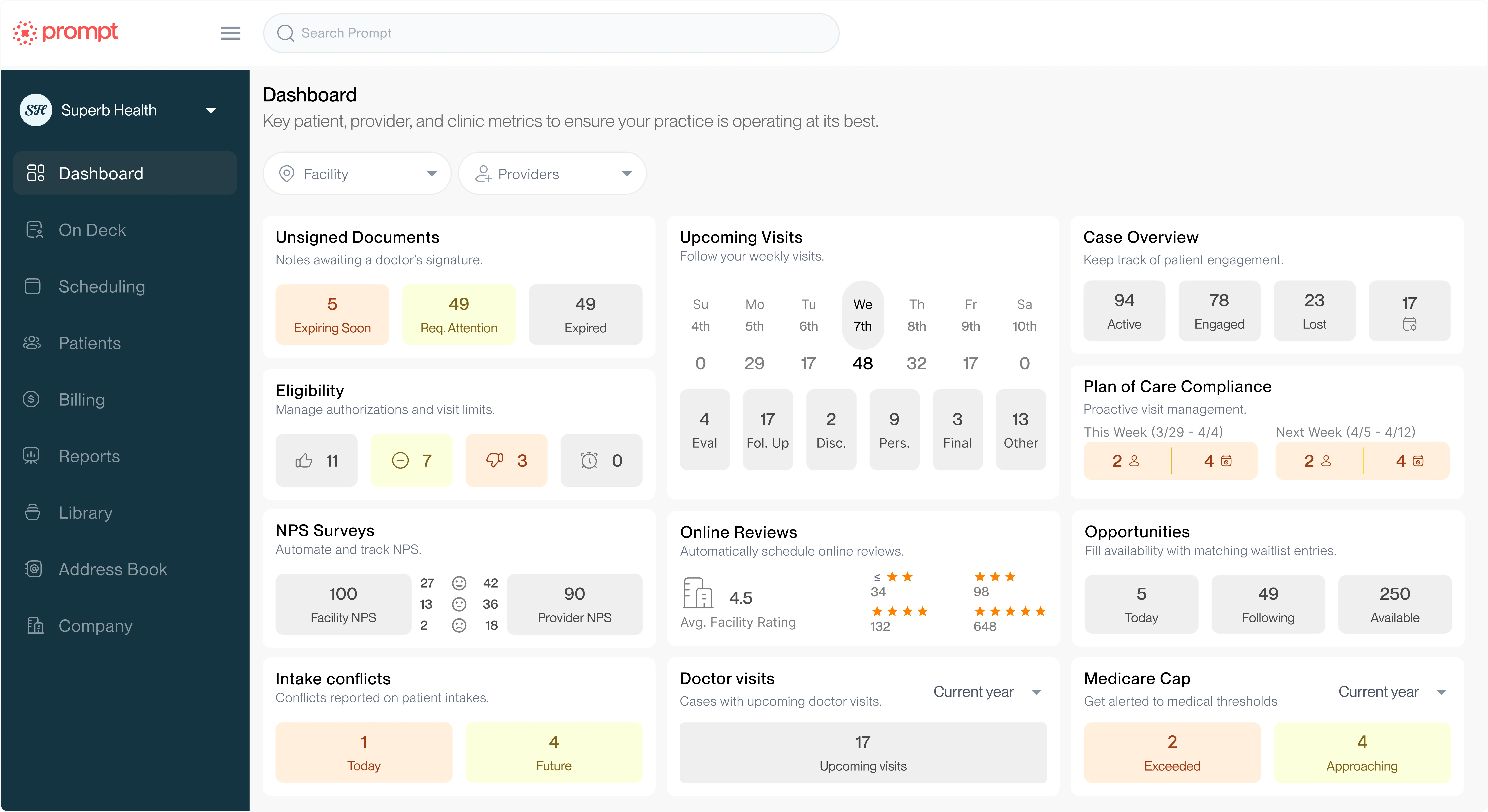
Prompt (formerly PredictionHealth) analyzed documentation and sign-off times across its user base to identify common documentation behaviors and understand how they might impact a clinician’s daily workflow.
What do all of these documentation personalities have in common? They all have inherent strengths and risks. Each documentation personality has found some rhythm to help them provide great patient care and complete the administrative tasks of being a provider.
Still, even the Methodical Organizer can be prone to over-documentation in an effort to be thorough in documenting patient care. And over-documentation doesn't equal better compliance and can sometimes even hinder it.
Documentation patterns that take place consistently after hours or even over several days introduce a higher risk of mistakes and errors as it becomes increasingly difficult to remember the details of a patient's visit, background, injury, and parts of the assessment with increased time between patient care and completing the documentation.
AI scribing solutions are relatively new but are growing in adoption quickly. Designed to alleviate the documentation burden and help clinicians reclaim their time, this technology uses ambient listening powered with AI to distinguish who is speaking, add context, and deliver clinical documentation from the provider-patient conversation.
While the basics of various AI scribing solutions are similar, several factors differentiate them, including:
In rehab therapy, AI scribing solutions vary in how specific they are to the industry and whether or not compliance and CPT coding help are built into the solution.
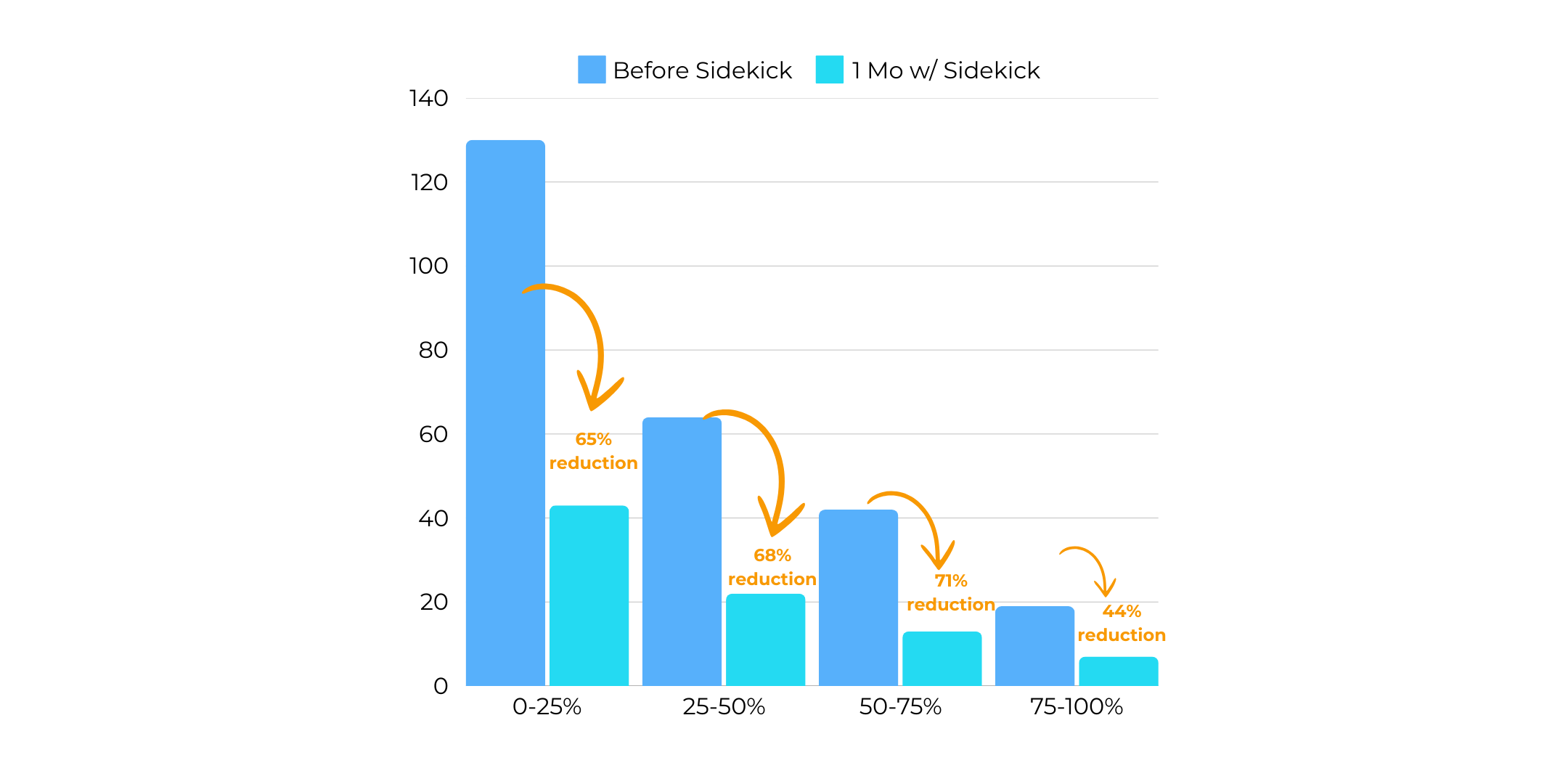
These are important distinctions because Prompt analyzed data points across its Sidekick user base evaluated changes in sign-off times, time-to-sign-off, compliance scores, and use of functional CPT codes.
These reflect significant outcomes for rehab therapy organizations as they impact not only burnout but also reimbursement rates and audit risk.
Without AI scribing, 50% of rehab therapy groups average more than 48 hours to sign off on patient charts, some seeing outliers that take over a week to sign off.
Long sign-off times and after-hours charting contribute to more than burnout; they drive lower compliance scores, too. When organizations used AI scribing (Sidekick) to document patient visits, the average hours to sign off dropped by 62% within one month.
Documentation compliance and CPT coding are critical aspects of healthcare, but they’re often viewed as tedious and complex. AI solves this by providing real-time insights and recommendations so clinicians can adjust their documentation behaviors without a learning curve or added burden.
For example, therapists may default to general codes like TherEx, even when interventions justify more specific functional activity codes.
An AI scribing solution tailored to this use case identifies these opportunities at the point of care, helping therapists code more accurately while adhering to compliance standards.
The results are clear:
These changes reduce audit risks and support better patient outcomes by emphasizing functional progress.
AI is reshaping how therapists approach their work and solving big challenges that previously strategies either couldn’t or were too resource-intense to sustain.
Tools like AI scribing demonstrate how powerful an ally technology can be to providers and leaders alike, reducing administrative burdens while improving compliance and coding accuracy.
To see these tools in action for yourself, schedule a demo today.
Help your practice grow
From intake to insights, Prompt is the all-in-one platform you need