See Prompt in action!
Spend enough time in a rehab clinic, and you will notice that clinicians document very differently, even when they work side by side.
When we analyzed documentation behaviors across thousands of rehab therapists nationwide, one thing became immediately clear: there is no single way they document, and the differences are not random. They are patterned, predictable, and very human.
Even better news: None of these patterns mean someone is doing a bad job.
They simply reflect how clinicians adapt to pressure, workload, and the systems around them.
Documentation habits don’t appear overnight. They develop slowly in response to real constraints in a clinic, like increased visit volume and decreased reimbursements.
Charting creeps into evenings and weekends and over time, therapists adjust in ways that help them survive the day.
The Prompt team dug into the data and analyzed signals like compliance scores, time to sign off, CPT code diversity, word count, and timing of documentation. When those signals were clustered together, 4 clear documentation archetypes emerged.
The Traditionalist is the therapist who takes documentation seriously. Very seriously.
They tend to have high compliance scores across the board. Their notes are thorough and consistent. Auditors rarely find surprises. But there is a tradeoff:
Our data shows Traditionalists take longer than average to sign off on notes, often well after the visit itself. Their CPT coding patterns are narrower, suggesting a preference for familiar and safe codes rather than exploring the full range of clinically appropriate options.
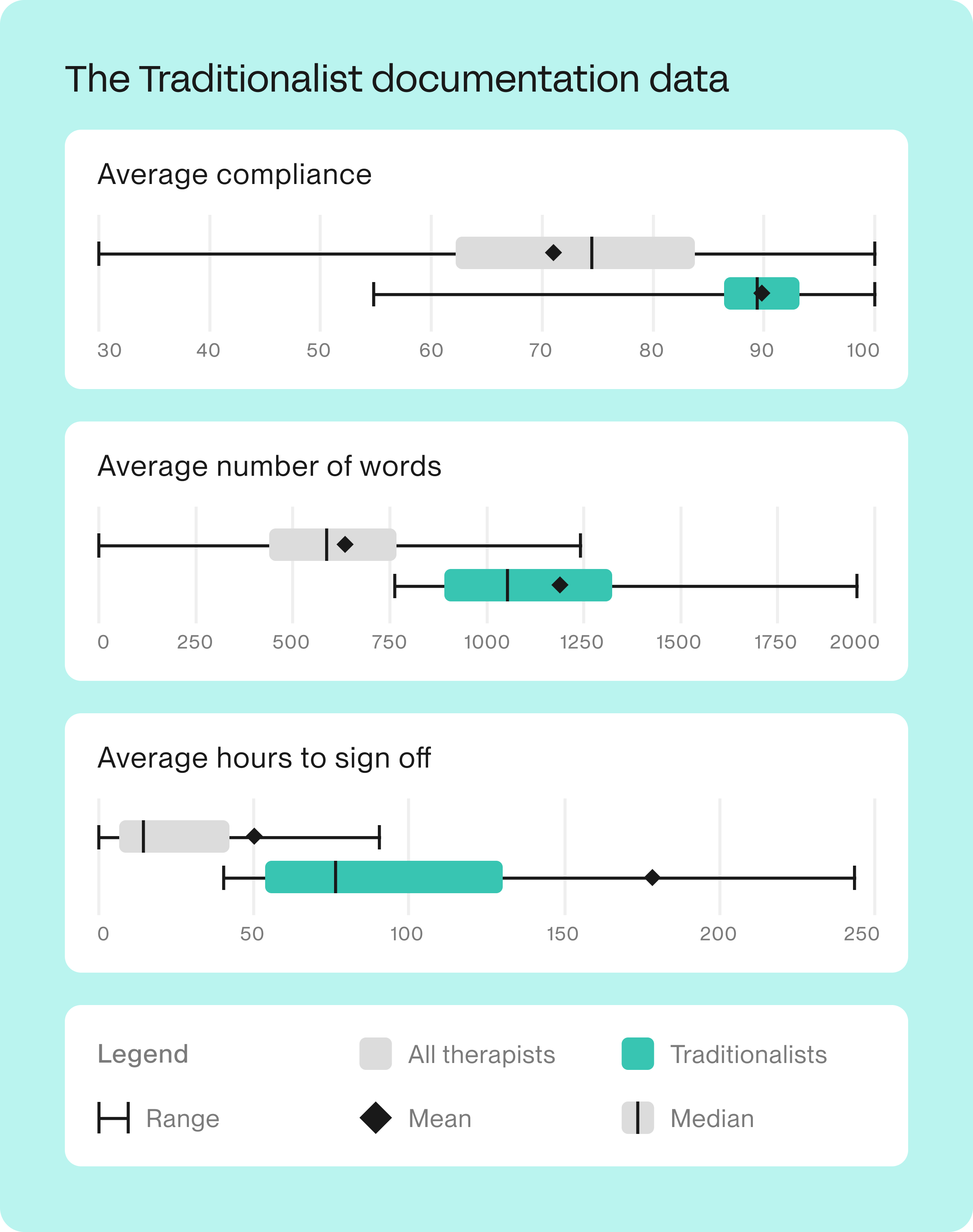
In human terms, Traditionalists care deeply. Sometimes so deeply that efficiency and flexibility suffer. They’re not resistant to change because they are stubborn. They are cautious because accuracy matters to them.
The Habitual Over-Coder is often described as operationally sharp. They know the codes, move fast, and generate revenue.
The data shows these clinicians use a broader range of CPT codes than average. On paper, that can look like sophistication. But compliance scores tend to lag behind peers, especially when coding intensity does not consistently match documentation justification.
Interestingly, this group shows higher disagreement rates with AI-generated CPT suggestions, which suggests strong confidence in existing habits.
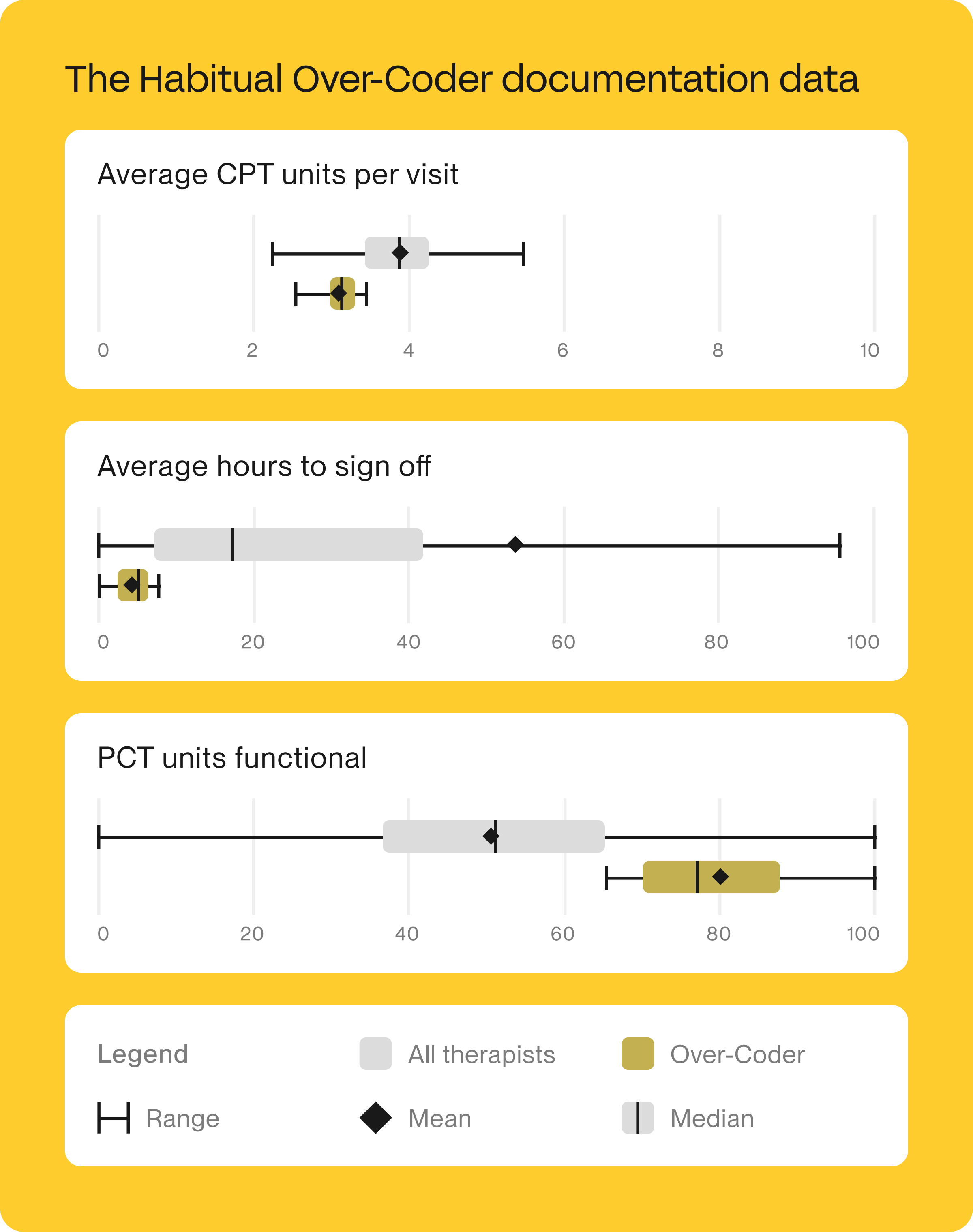
Over-Coders are rarely careless. More often, they are trying to keep clinics running under financial pressure. Their habits worked once, so they stuck. And while Over-Coders think they’re helping by being diverse with their codes, they sometimes can actually be contributing to audit risk for the clinic overall.
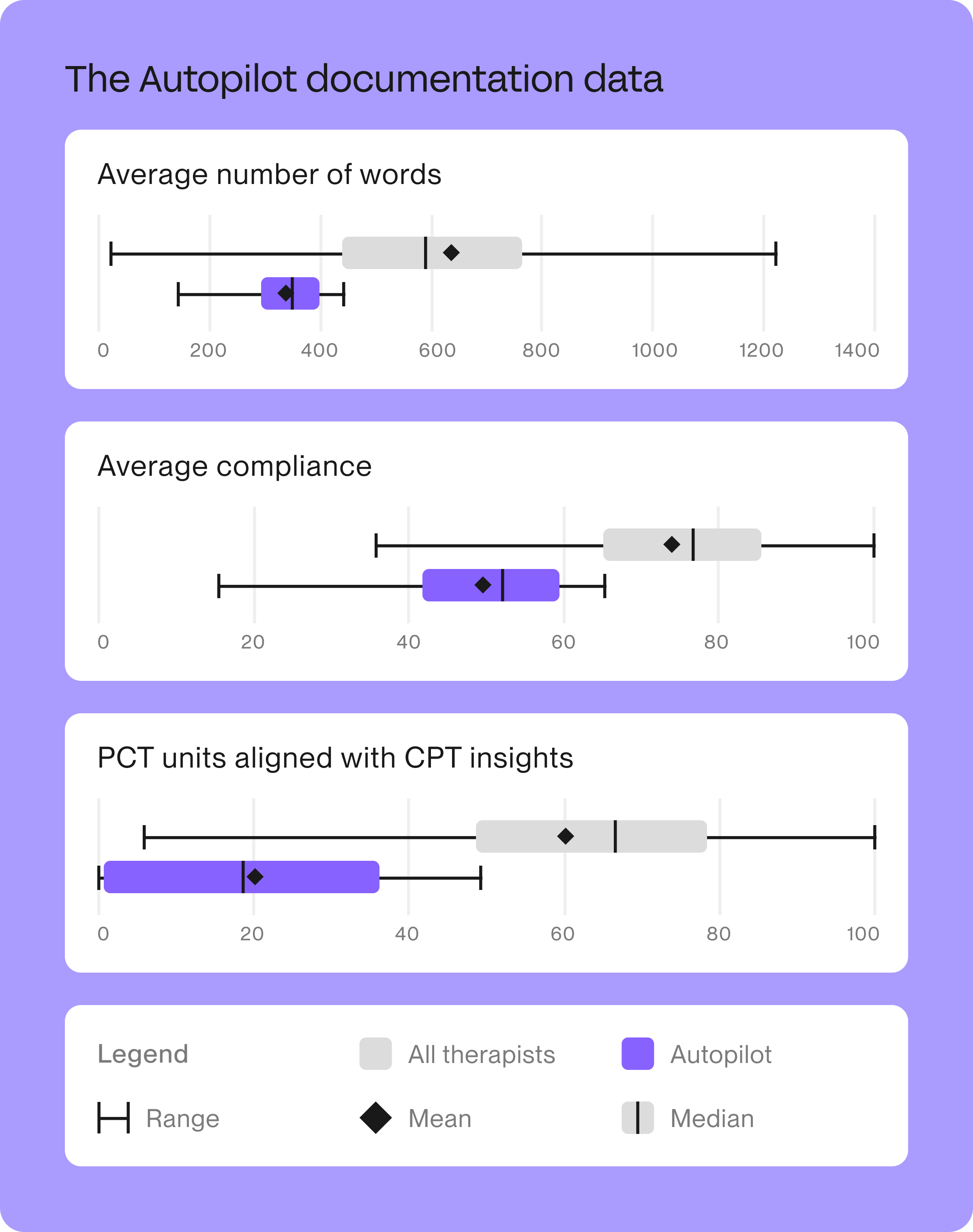
The Autopilot therapist is fast. Notes get signed quickly, and their documentation rarely spills late into the evening.
But when you look closer, the documentation itself is thin.
The data shows low word count, low functional unit usage, and lower compliance scores overall. These clinicians tend to perform tasks efficiently, but without much narrative depth.
Autopilot mode usually appears when clinicians are overloaded. It’s a way to protect time and energy. Unfortunately, speed without depth can quietly create risk.
The Treadmill therapist never stops moving.
They see a high number of visits. Their documentation often happens late at night. Notes pile up, then get cleared in bursts, only to pile back up again. They’re running in place. The data shows this group has higher patient drop-off risk and a strong correlation with delayed sign off times.
This isn’t a motivation problem: it’s a bandwidth problem.
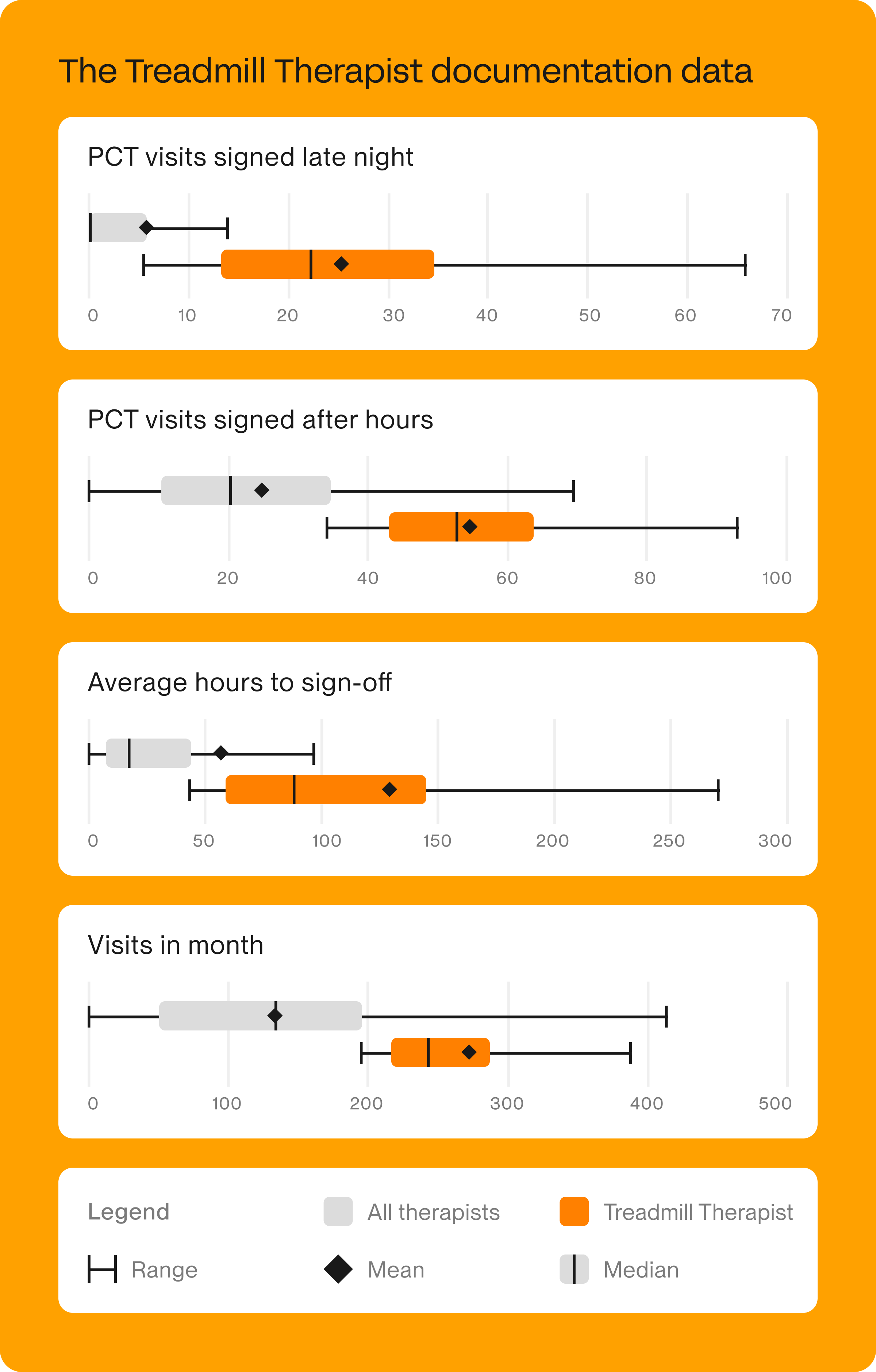
One of the most striking findings was how much this group benefited from workflow support. When documentation burden eased, compliance improved by double digits and late night sign offs dropped significantly.
Though it may be tempting to focus on the challenges of each archetype, the reality is that every archetype exists because it solves a real problem:
The risk appears when systems treat all clinicians the same and expect one solution to work for everyone.
Generic compliance training assumes everyone has the same problem, but they don’t.
Retrospective audits punish outcomes rather than guiding behavior in the moment. Policy updates change rules, but rarely change habits.
The data shows that improvement happens fastest when support matches the therapist’s documentation style.
For Traditionalists, the biggest concern with AI is usually trust. Accuracy matters deeply, and anything that feels like a shortcut can raise alarms.
The data is reassuring: When AI scribing was introduced to Traditionalists, they signed notes faster without losing compliance or coding integrity. Word count dropped slightly, but compliance scores held steady and coding diversity did not decline.

The reason is simple: Ambient listening and real-time dictation reduce the mechanical burden of writing without taking away clinical judgment. The therapist still controls the final note, but the path to completion is shorter.
For Traditionalists, AI works best as a quiet assistant that handles structure and transcription, not decision-making.
Habitual Over-Coders tend to have strong opinions about coding, and for good reason. They’re often responsible for keeping revenue healthy in challenging environments.
The data shows that when AI provides CPT guidance at the point of care, compliance improves meaningfully for this group. In some cases, time to sign off increases slightly, which is not necessarily a bad thing. That extra time often reflects more thoughtful alignment between documentation and coding.
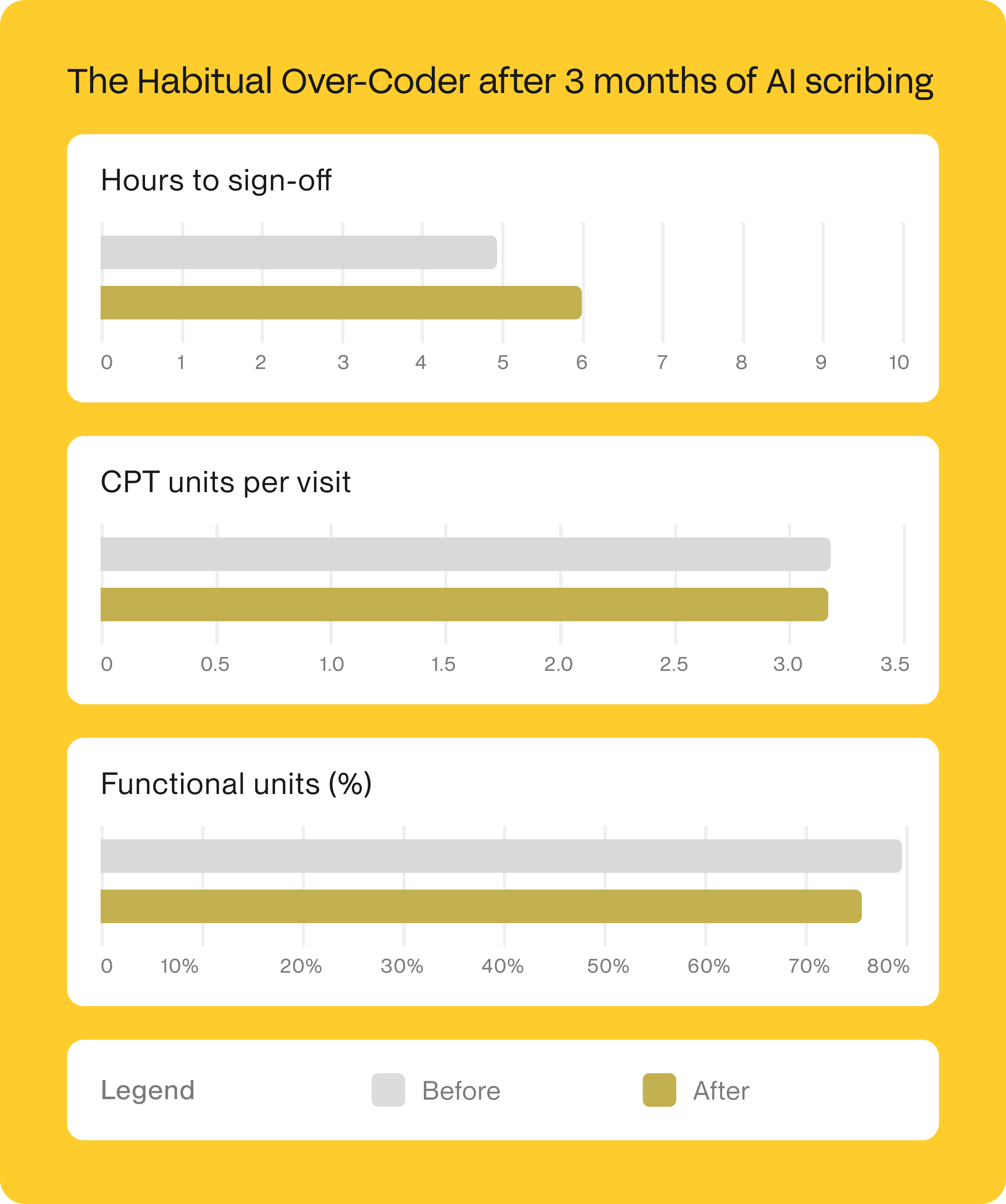
Instead of correcting habits after the fact through audits, AI helps introduce small course corrections in the moment. Over time, those adjustments compound into better compliance without sacrificing productivity.
For Over-Coders, AI is most effective when it supports their own judgment, rather than replacing it.
Autopilot therapists value speed and patient focus. Documentation is something to get through, not linger on.
When AI scribing is introduced, this group shows one of the most striking improvements. Compliance scores increased by an average of 16 points compared to the broader population. CPT coding diversity also improved, which creates higher reimbursement potential without adding work.
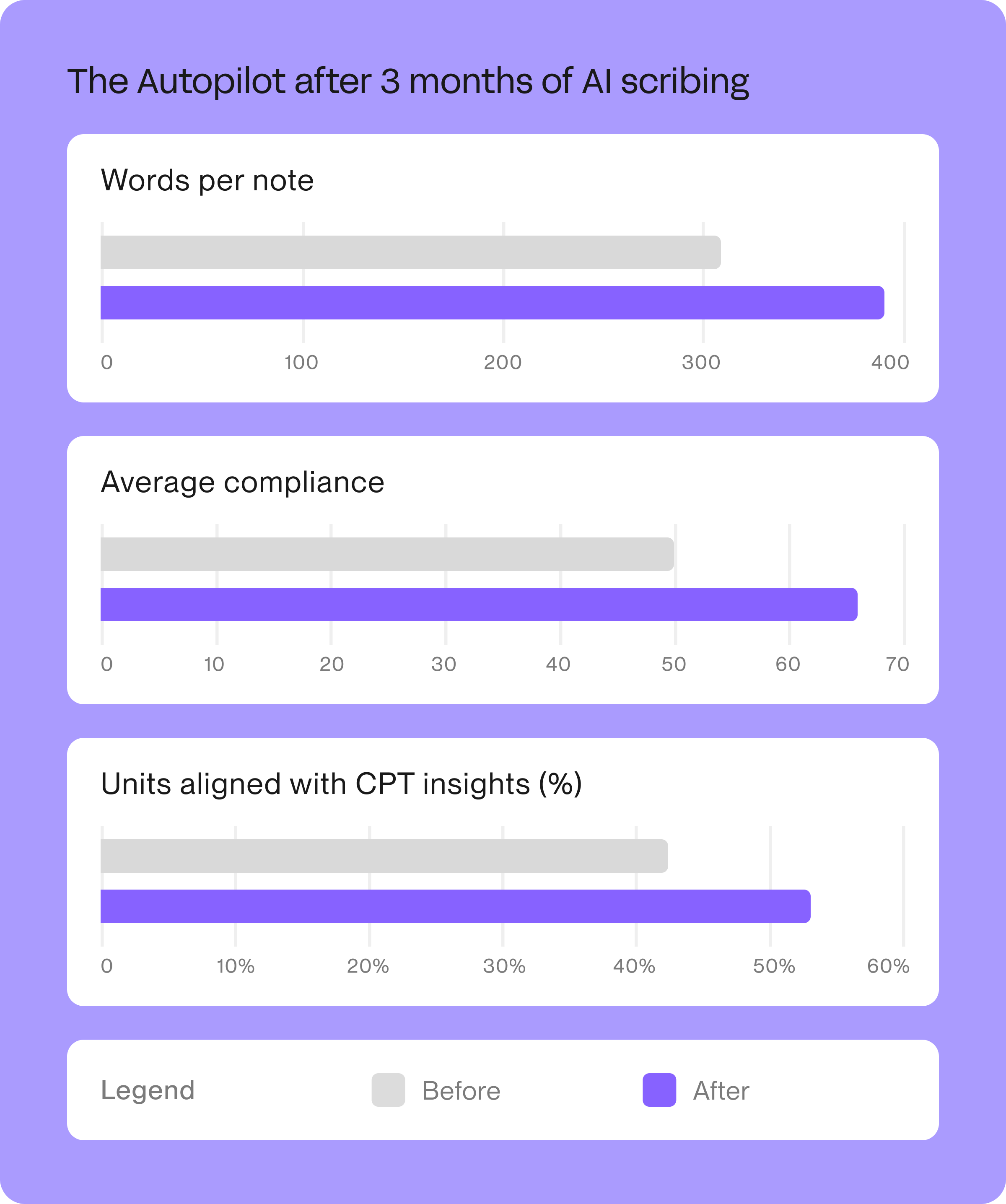
The key is that AI fills in narrative detail automatically while clinicians continue working at their natural pace. There is no added documentation step and no need to slow down.
For Autopilot therapists, AI adds substance without asking for more time, which is often the only sustainable path to improvement.
Treadmill therapists experience the heaviest documentation burden, and the data reflects that strain clearly.
After AI scribing adoption, this group saw more than a full day improvement in time to sign off. Compliance jumped by over 12 points, and late night sign offs dropped by 21 percent.
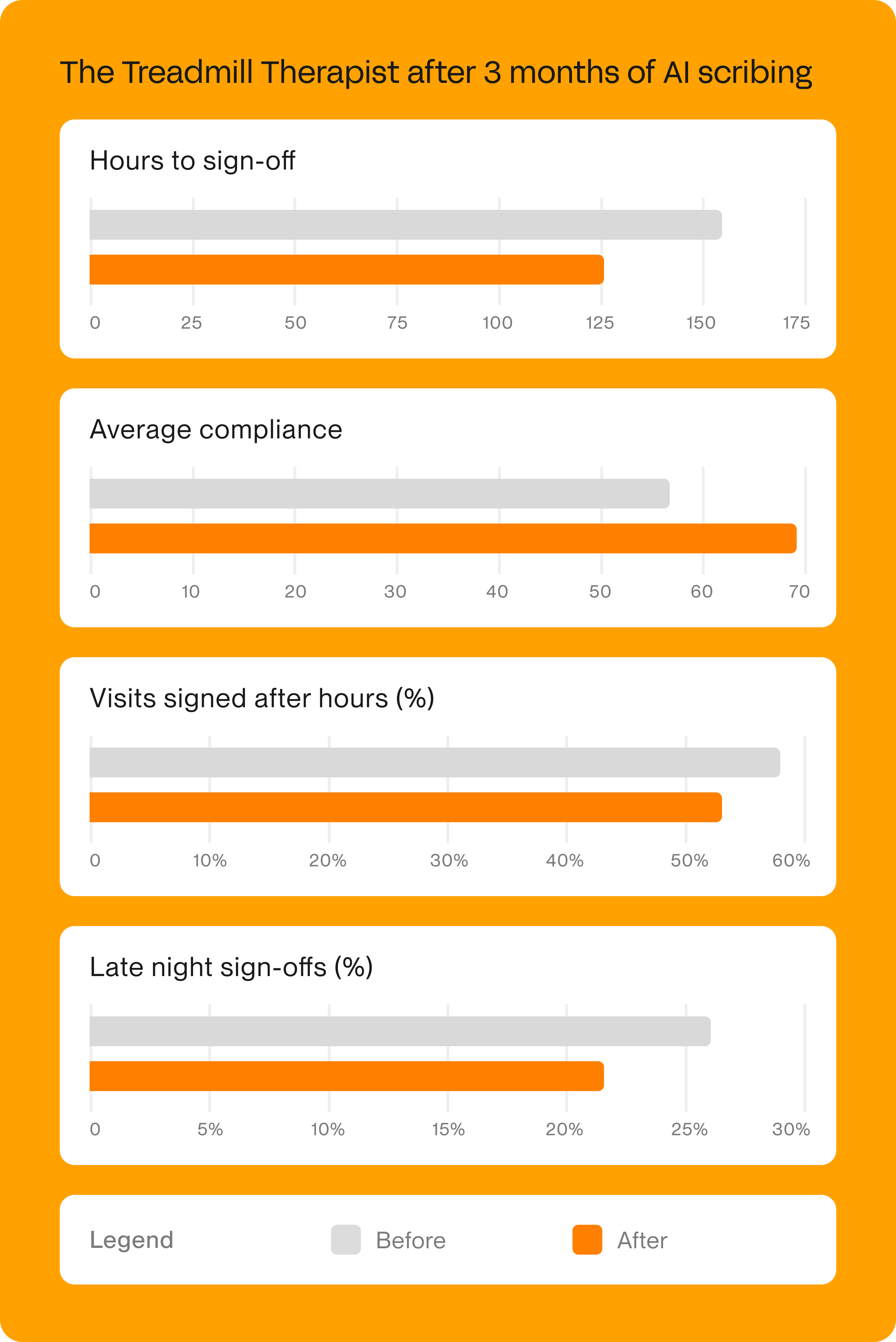
These changes matter because they interrupt the cycle of backlog and burnout. Documentation happens closer to the visit. Cognitive load decreases. Evenings begin to feel like evenings again.
For Treadmill therapists, AI isn't about optimization. It’s about sustainability.
Across all 4 archetypes, the same pattern emerged: AI worked best when it respected how clinicians already function.
No one had to become a different kind of clinician. The technology adapted to the behavior, not the other way around. That’s why the improvements stuck.
When leaders stop asking “Who is compliant?” and start asking “How do our therapists adapt?” everything changes.
Documentation becomes less about enforcement and more about enablement. And clinicians stop feeling like they are failing at paperwork when in reality they have been succeeding at survival.
To learn more about how AI scribing can help your documentation, schedule time with one of our Sidekick experts today.
Help your practice grow
From intake to insights, Prompt is the all-in-one platform you need