Book a demo

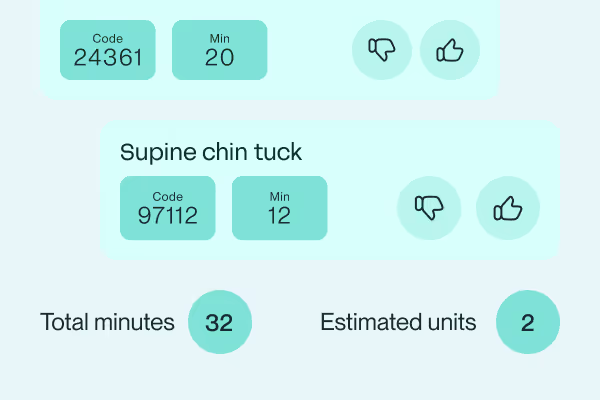
AI identifies coding errors and highlights denial trends with recommended actions, while Appeal Packet Management pre-fills payer forms and documents so staff can resolve denied claims quickly.
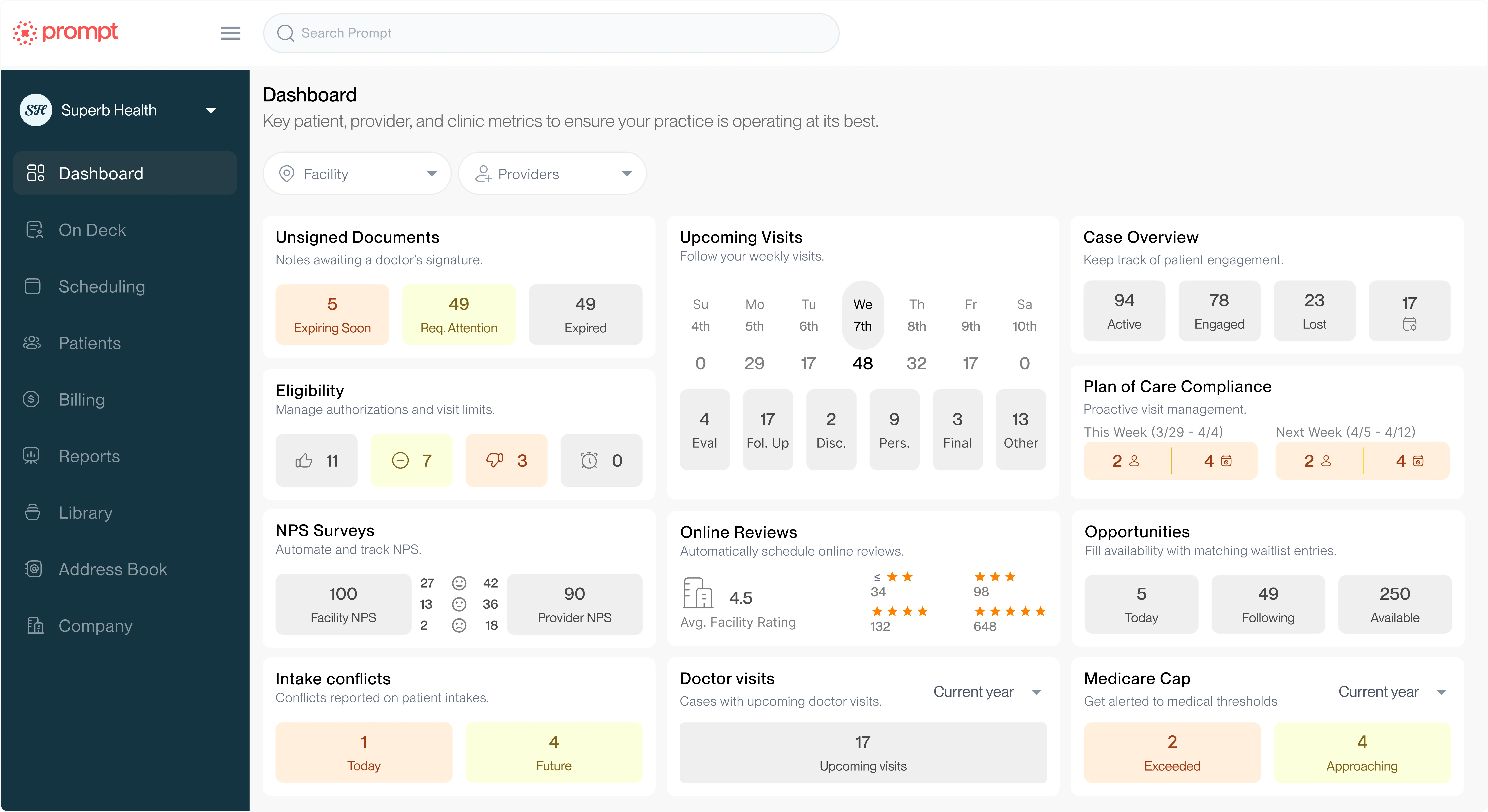
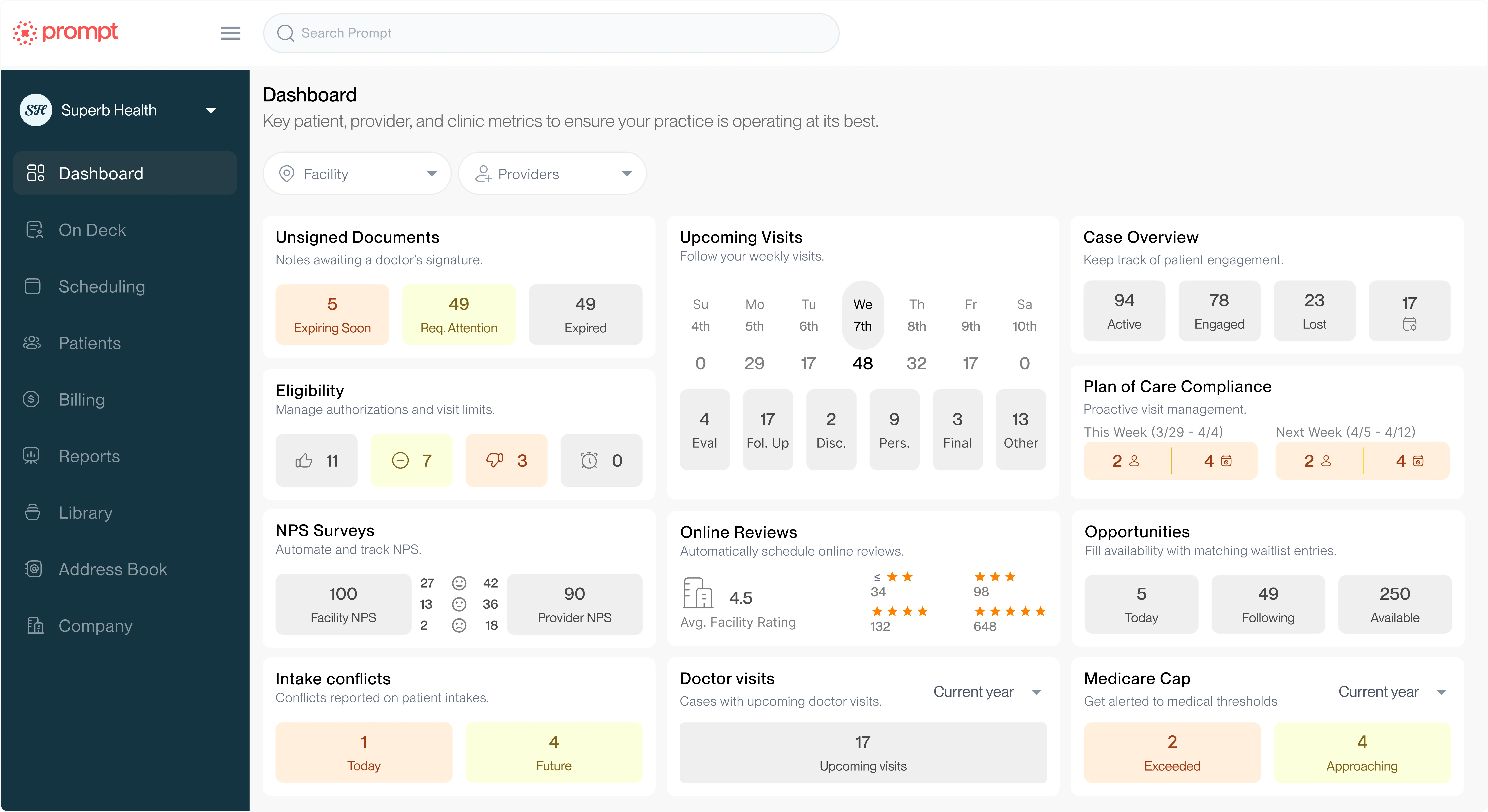
Track and trust your key billing KPIs with accurate expected reimbursements, variance alerts, hard period closes, and reports showing remits, payments, and claim activity.
Process claims smoothly with full visibility of payer responses without leaving Prompt
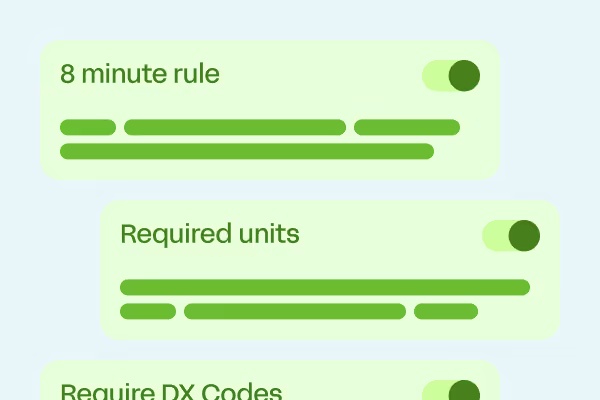
AI handles 90% of the work, leaving you to focus on the claims that actually require human intervention. Upon checkout, Prompt:





Prompt has allowed us to make billing extremely efficient. We have 10 providers and 1 biller currently working on our claim submission and AR. Thanks to Prompt, it's very streamlined.
Learn about these additional capabilities and how they can help your business grow and thrive