Transcript
Justin: Hello everyone. Welcome. We're excited to have everyone here today. I just wanna kick this off and do a little bit of housekeeping to start us with and just to let everyone know that the chat is open, so if you guys wanna use it to say hello or share anything. You can do that throughout the session.
There's also a q and a tab, so if there's any questions that you guys want in there, you can drop 'em in there and we'll make sure we take care of those towards the end. And then last but not least, this will be recorded and sent out to everyone, so don't feel like you need to take too many notes and you can just play along and ask questions throughout.
And we'll send that recording out after that. And then I will start with just some basic. Productions from everyone here. Starting with myself. I'm Justin Ferguson. I work here at Prompt. I am a senior director over our RCM services, product and support section. And also help with our strategy there.
And then I'll pass it over to Josh Grover real quick.
Josh: Yeah. Hi thanks everybody for being with us and thank you panelists for coming here and being able to talk with us about this. My name is Josh Grover. As Justin stated, I work here at PROMPT as well. I'm a director of CS Small and mid-market, and I am also currently standing up the coaching division at Prompt.
So where we can do a little bit more white glove with exactly the things we might talk about today. And I will kick it over to Phil.
Phil: My name is Phil Firkins. I own four physical therapy clinics in the Pittsburgh area. We've been with prom for about four months now. Helped onboard some of the AU and VOB as well, so I'll push it over to Ken.
Kendra: Hi, I am Kendra Broman. I'm the Revenue Cycle director for Go Physical Therapy, and then we also have a billing company called Powerhouse Billing. So that's what I'm representing today for the RCM side of things. So excited to be here. We have been on prompt for about 15 months,
Justin: amazing. Thank you everyone.
And the idea today is just to have a very conversational session with our panelists and also with the q and as. Whether it's billing on prompt, just billing in the therapy industry in general and some just hidden and inefficient workflows that people have a uncovered, whether it's.
Switching EMRs, billing services again, even bringing billing in house. So we're gonna go through and just talk about different experiences and again, keep it very conversational. This isn't just one one piece, just like if it's outsource billing or also just within the product. So we're gonna start with going over the hidden cost of a inefficient workflows and just ask a couple basic questions regarding.
Really like different workflows that you either uncovered through an EMR transition, transitioning billing services that you un uncovered that was maybe inefficient costing you money that you didn't even know was happening. And so I'm gonna start with a question of what did your workflows look like before upgrading your system as our two panelists?
Recently and then about over a year ago, went over to prompt. And what kind of problems were you running into?
Phil: So this is our third transition in EMR and RCM platforms and a little shy of four years anymore will probably lead to anarchy. So we changed from one legacy RCM that also EMR, that also did RCM.
And we found that when they were linked together, the EMR tended to be the priority and we noticed scaling AR DSO being a challenge. So we did bifurcate. MR and RCM platforms and then noticed that communication between the three parties of our clinics, RCM and EMR became a challenge. So another franchisee in our clinic and our franchise introduced us to Prompt and we were sold on the team based approach, which is how we run our clinic too.
Found good carryover in that and found, kick up in the revenue and the lack of time spent. Non-billable, time spent chasing leads, which is non-billable time is a tough sentence to say, I think in our world with some of the struggles that we have as clinic owners. But again, I'm four months in, but it's been fun to be part of the team.
Justin: Has it been, have you experienced any kind of challenges? A lot of people, I think when they're making the switch, not only in EMRs but also the switch in a billing partner I think a lot of people worry about that transition period. How have you felt like being at the, just past kind of 90 days has it felt have you had a major dip in revenue?
Have you had any major concerns with communication and getting everything to flow into the new system and how have you approached that and felt with that so far? Pre go
Phil: live is, was terror because I think that there's a lot of trust involved, getting paid for services rendered and we had, we have, with all the challenges with Medicare reductions and reimbursement, all the challenges we deal with in this world, write offs, progressive DSO and AR was a challenge since go live.
None. It's been wonderful. I know who to go to, email, text, call for RCM. I have one point of contact, so we'll get it done. She's sweet too. I have same thing with author VOB, which has been a fun thing to help pilot. We sadly had to staff two clinicians at home hours between four and eight hours a week to try to help our legacy RCM platform kind of chase challenging leads, which.
They now don't have to do, and they want something else to do at home for those hours, but we have not, we haven't been able to cut that. But the communication's been great. We have one person, very responsive, whether it's internal in the system, emails, calls, texts carryover communication's. Been solid.
So I'm,
Josh: I'm curious in, other systems, A lot of times when I go into a clinic and ask some questions or look into things, there's a lot of times where they're chasing ghosts is what I like to call it, is basically, they're, they don't, the data integrity of the purports, they're pulling they're spending a lot of time chasing down accurate data because the native ports, they were pull they're pulling might not be accurate or when they.
Do their own manual testing on it. It's we're not getting the same numbers here. And so now they're just paying people to essentially, see how the data integrity is and then figure it out very manually. Did that change for you? Did that happen and then did that change for you at all when you
Phil: made it?
It happened in many ways. I think chasing ghost is a polite way to put it, wasting time. I could come up with several others. We have, we had many challenges and. It became an issue when our DSO got to a point where it was like 35% of what we gross in a year was outstanding. And a good chunk of that was six months, 180 days, 365 days outstanding.
And we finally, which I'm, I don't love to be pushy and shabby, but got higher ups on these calls, which again is now my. And my business partner's billable time or we're on calls once a week for two hours chasing any lead beginning at 90 days and prioritizing anything beyond 180 days. And I, I just, I remember the first call we had where, alphabet alphabetical order was great, first patient was discharge discharged 14 months ago, 27 visits outstanding.
And they can go through in the software and see the last time that any. Any pursuit was made on that account and it was more than six months. And it was work comp patient that just needed transition from work hardening to work conditioning. And we had three emails sent complete. That was the ghost was the communication in response.
I don't love getting ghosted anyway, but we had made the the attempts to get there in 27 visits. Over that period of time we finally then waste our time, chasing, go see her on this call, and they've all been paid since then. But it became two hours every week, more than just myself from our team on the call, and then needed to get higher ups on every call to make sure there was carryover, which was, it's just unnecessary mud and water.
Josh: After the switch, did you see that clean up
Phil: a little bit? You saw? Very much yeah. Our revenue is actually I just got my data for month to date and we're up $8 and 54 cents from like our trailing 30 days as opposed to our trailing nine months pre go live. So without paying clinicians to work from home to chase this without doing these lovely two hour calls every Wednesday at noon.
And everything else. So
Josh: I can imagine that made forecasting pretty difficult. Which caused probably a lot of angst and anxiety amongst you guys.
Phil: It throws on, incalculable variables into the mix with regard to, and then not, there's things that are budgetable, like budgeting hours from home that we can work into our numbers, but the.
When you become numb to write-offs and to yeah. Six plus figures one year outstanding that have not been touched or communicated upon, and you get numb to it. I think that can be a scary thought. I think that was where we finally got higher ups on the calls because it just became part of life, which is I think, a little worrisome.
No, nothing changes when you get numb to it. So made change.
Justin: Kendra, what are some things that you've noticed? One, having a billing service that utilizes heavily on prompt and then also with GO pt transitioning over the last 15 months. Onto prompt. Obviously I know like I've worked with you as your billing success manager, and then.
But just as like a colleague in the space too. What are some of those kind of big C cha not even challenges that the inefficiencies you recognize switching over. I know you guys did more of a phased approach too with the different brands in different areas. What was some of those first past things that you noticed?
Yeah.
Kendra: We noticed actually lots of things, but we have 19 clinics for Go and it, we did roll it out in a phase approach which actually worked out fairly well. I think it's got us used to the system, got all the things, the rules we wanted set up. But the big one for us is because of our volume.
It's really easy to get lost in all of the claims. It doesn't take long and you're just, there's just so many claims and the team's just swimming and how do they know what to tackle and it's really great that you don't have to. Run reports to figure out where those maybe loosens are, or ghosts maybe that need to be chased.
You're able to slice and dice it within the billing platform to drill down to, okay, what's outstanding for last year yet? What's going on with this location, what's going on with this payer? And really get down to the. To the issues right there within the billing system, and anyone on our team can do that.
So it makes our billers work smarter versus harder. I know we talked about this a lot and one of our big things for my push to prompt was automation of payments. Nothing drives me more crazy. Where if the claim's clean, why does anyone have to touch it? If the payment's clean, why does anyone have to touch it, legacy systems, you still had to touch all those payments and just seems like a waste of time when if it's clean let's have it auto post and so we could set up all those rules by the payer and nobody even has to look at 'em. 'cause we want our team spending the time where we need them to spend it.
Insurance companies are not making it easier for us. So we need to spend our time on the claims that we need to be spending 'em on.
Josh: That's a great point. Kendra is like getting rid of some of that redundancy, which is touching clean claims, is very redundant, right? And it leaves no time for the team to be reactive or creative in the next steps that they could be doing something that need moves the needle even more.
I, they're bogged down in like this tedious task of just doing redundancies. Happy to hear you. You saw that clean up a little bit and able to negate those
Kendra: Yeah, exactly.
Josh: Things. Yeah,
Kendra: Yeah. Because with those payment, with the auto payment posting, before you're posting this giant payment with all these clean payments, everything's watered down.
And now we're only looking at the problems. So it's much. Easier to identify issues right away. Yeah, we won't name any specific payers, some payments come in and half the denials on that remit are for one reason right away. There might be an issue we need to dig into or communicate with the payer on.
Josh: You can action on 'em so much faster, right?
Kendra: Right.
Josh: Crazy, right? I always liken it to the analogy of in some of the other systems I've been in or seeing it's like walking in a dark tunnel with this very small flashlight and then prompt just is like this giant spotlight behind you, right?
And you can see everything, it's almost in your face. So you're able to action those things very quickly. There's nothing hiding, so to speak, really anywhere. So it's, yeah, it's great.
Justin: I think that's another thing that I didn't even really realize until I came over to Prompt and then as we were building out the RCM section too was a lot of the legacy, whether it was EMR companies I worked with even also third party billers is we were working in a separate practice management system outside of the EMR.
So a lot of it had a compendium, it would transfer information over. And something I never thought about on being like the actual biller on that side was the visibility from the clinic owners and the clinicians. Because it was a separate system. So a lot of times what they were getting insights into were reports we were offering them.
But within prompt, and like especially it all being a true, like all in one software, it's all permission based. And I think like being able to actually go in there and see. What is actually happening? Like I can see the last time a claim was action done, I can see exactly where it's sitting.
It's not me just trusting a report someone's sending me. And like able to like actually go in and just, I can, I have full visibility. There's no permission access or anything else that I need to worry through. And I'm not hosting multiple systems like I used to have to reconcile from the EMR to the PM system and make sure the copays and everything came across.
And having it all truly on one encounter is it's been a game changer too for myself. Let's see if there's a question on here. It looks like someone asked a question, Kendra, this would be a good one for you too, is just what steps did you take to set up the auto poster? I think that's something we even talked about just yesterday, but it's with the auto poster, there's a lot of different granularity and levels and I'll like Kendra add to this too, but I think a lot of people start with the most, what we call conservative version, which is just the basic settings.
It pretty much is gonna stop more than it's gonna put through. And then my usual recommendation on the billing success side when I'm teaching customers how to use it is. Every time I have a payment come in that I have to just go manually post, I take note of it and like why I'm posting it.
Was it just like a adjustment code that's not something I can go get money on? Is it a per diem payer that is gonna pay me like a set rate and they're gonna adjust off the prior codes even though that's not a denial. And what I do is if I write that same thing down like three or four times and it's, I'm doing that same action every single time, that's typically when I start trusting automation and I'll turn it on.
I don't wanna go too fast and do it because maybe that's like an edge case that I actually do wanna look at sometimes. So I usually have people make a rule of thumb, if I'm doing this 95, 90 8% of the time, let's automate it. And you can turn those on either at the payer level, like the individual payer level or the payer class level too.
Is that the approach you've taking Kendra?
Kendra: Yeah, Justin, you know me better than anyone here. I'm a control freak, so I have trust issues with this auto posting. But so we did, we, we turned it on, then we did some audits on the back end and make sure it was doing what we wanted to do.
And it was, and then slowly, like you said, you can add those more strict rules and, when we're training a new poster or anyone that's gonna start learning the posting, the first question you ask yourself when you're posting that payment, why did it not out post? Could it have auto posted? Do we add need to add a new rule?
Do we need to work with the prompt team? Because kinda what Phil was saying earlier, we do have built great relationships and we're able to dialogue back and forth with ways we can make the product even better. And so if there's things that we need to maybe work with the clearinghouse on, like it's, we can open up those discussions.
So that's what we always ask first is why is it not out of posting? And maybe it's legit. Okay. The payer, has an issue, then we'll move on. But there's things that we find, pretty often that we're able then to turn on, whether it's a specific code for certain payers. But we've also turned off auto posting for payers, like some of those crossover HRA that you just can't catch 'cause the patients don't tell you they have that insurance.
And then, so to avoid those issues, with the patient getting a wrong balance, we've turned off auto posting for specific payers for some of those rules.
Phil: Absolute thanks. Speaking on the payer roles, if any here aren't familiar, that's been a life changer for us because on the clinic side, I don't know as much of what all you guys do had trust issues as well.
Good on that. But I like that with my team, that we can control and make sure. Again I think Josh used the word redundancy a lot. The redundancy of, sending the wrong code for e-stim for the wrong payer, so I can go in that payer, change the role to only allow, the certain code that is reimbursable to be billed.
So now we're not waiting 30 days until that's caught getting, then waiting 30 days for them to pay. It's just they can't sign it if the incorrect code is on there and we can make that payer specific which is efficiency. Is a great word and it's really helped on the efficiency side of that as well, on a team level clinical level.
Josh: That's a great point, Phil. And it also reduces mental load, right? Like with the clinicians, they've got so much they gotta worry about whether when their patient like focused worrying about what they can and cannot add to any singular payer and keeping that in their mind is not something anybody wants to be doing.
So I feel like. And this is what we strive for at prompt, right? Anything we can let the system handle for you guys so that it's strictly patient focused, is what we want to do. So those payer rules come in big time. I feel like with that.
Phil: I'm gonna tag onto Kendra and say, I'm a control freak too.
Every one of our clinicians at every site I made a billing bible, I called it, where it's six laminated sheets, payer specific commercial, federal, personal injury, et cetera. Max those that involve, we'll only reimburse four codes. Those that have. Apply code X or code Y.
And now I have a little sentimentality to it, so they're not allowed to throw 'em away, but we don't need to really use those anymore. We'll touch and go with that. But it's good to, to trust it on here. Instead,
Justin: I, I need to do the same thing. I, we had these little Excel template, like no cards, and it was like, if it's Blue Cross, here's the rules you should follow.
Exactly. And you have different little, the cheat sheets. And it's nice one to have that. Stored in your system, right? And you can audit it a lot quicker. Everyone has access to it. But I think the other thing is providers, they're, I think the number one goal is treating the patient, having a good patient experience and taking care of them is, you wanna know what you're doing.
You're signing off on the note, you're signing off on the charges, but at the same time, those aren't, you don't have just codes in your head all day that you're thinking like, let me add a 59 modifier to this. Let me do this. So I think having the system proactively prompt you to say, Hey, this is what you should be doing.
But you can also have they call 'em tool tips in there and it can say why. And I think that's always nice for especially newer providers when they're in there and they're just like hitting all these buttons. It's what am I signing? What am I like trusting, giving visibility, but at the same time.
Helping them guide them to the next steps. And as everyone said, payers aren't making it easier. So like, why can I do it for this commercial payer but not this other one? And having a nice streamlined like stack in the EMR to tell you like, Hey, these are the rules we need to follow. It really helps downstream too on the RCM side.
I think in a lot of legacy systems you catch those with like EDI edits or they call 'em soft rejections which people don't recognize. Yeah, you're still getting it done before it gets to the payer, but at the same time, someone spending time to send that rejection back to the provider to make the change before it goes out again.
And that's all, again, non-billable, wasted time. So anything you can get to have that first pass, go out and get that payment clean. Lets the. The therapist focus obviously on the patients, but then the billers get a focus on like actual revenue they can recover. All great points.
Alright, let's.
Josh: Yeah, so I think we are moving on to the billing and coding errors now and just, some of the biggest revenue drains there that we can encounter. I always like to say too, whenever we went into a clinic to help refine their processes and help them just.
Kind of fix some of those small little things that are revenue leakage. It's never like this big monster that I open up the closet and oh, there's your problem, there's all your revenue, right? It's these little revenue leakages all over the place. Just tiny problems that when you start plugging those holes, next thing you know your margins are up a little bit and then a month later, a little bit more.
And a lot of that stuff comes from. Just those common coding errors or common denials that we see over and over again. And again, we're just blind to 'em sometimes. So having transparency to see those certain things, I think is a great way to again, just improve all the processes, essentially, having your billing and the transparency there help build out your operational processes, right?
Like we know two thirds. Of denials in the industry come from upfront right from the beginning whether that be through just EMB checks, which I know Phil, you've opted into here with us. Authorizations or just even demographic issues, right? Like putting in the demographics incorrectly. Then there's a whole bunch of tools, impro, and we can.
Get to those, but I'd love to that help with that. But I would love to know, Phil, like what did your revenue challenges look like before improving the billing processes? Here with Pro the prompt switch.
Phil: If I had to dumb it down to a couple things, 'cause I could speak on that prior for the remainder of the hour.
I think the trust in carryover, again it's getting paid for services rendered has become the hardest part of any level of ownership in healthcare as has been mentioned. I think four times they are not making it easier. They change prior to telling you they change. And communication.
So I, again I needed something about 30 minutes before this call sent a text and I got it about four minutes later. Communication has been, just, has been great. There's been no reason not to trust the process at this point. Transparency, all being on one system has been great. I know we were pushy about onboarding the author and VOB stuff too, to try to keep that all in template in the system, which, I, we agreed to sign on to and work through the bumps a little bit if there were any, because we were already staffing people to work from home to help with the process.
If we were already helping in that process, why not continue to help in this process just to make sure it goes smooth? And now they're already out of the work from home stuff, so we gotta come up with other stuff, but. Communication and trust has been big. We get our big fancy financial report at 120 days here next week.
So I'm excited to see what that, I got most of the data now, but excited to see the rest of that at this point too. But we've already seen an untick an uptick in our KPIs, revenue per visit, et cetera. And some of that's just cutting the fat. With regard to waste of time, unbillable time, which in a world where margins can get as pinched as they can in outpatient healthcare unbillable time is sin.
So it's helped.
Josh: And pri, prior to your switch, what do you, if you do know, I would love if you would care to share with us, do you know what, like your bigger, biggest denial points were? What was. What the issues were, those denials and then have you seen that get better after your switch? Your denial rate and getting rid of those things?
Phil: Yeah, a lot of it was, again, back to the challenge of the payers. I think the lack of, our. Our vintage EMR or RCM platform would just go on the website. They wouldn't really, they chase the low hanging fruit, but we would get incorrect information on whether auth was required visit at max whether there was copays.
And I think trust isn't just between, R-C-M-E-M-R and clinic owners, but it's. If we're a consumer facing product to the patient, and we had this happen so many times, and they're the most uncomfortable conversations, when you see a patient for 20 visits, who you have them sign has a $0 deductible, no authorizations, and then you have to tell 'em yeah, you actually have a $2,000 deductible.
Here's your EOB. It is uncomfortable. I know we're 105 days into this, but we have not had any of those. A lot of it was just. Not carrying over and just maybe expecting that every Highmark senior health plan was the same and they didn't require authorizations. And then we now are the individuals who speak to the patient and or just write it off to avoid the freaking conversation to a point which was done more often than not.
So that has been wonderful in carryover. I would pay anything to not have those conversations, and we have not had one yet,
Josh: yeah, those authorizations, I call 'em clinic killers because you can't get them retroed, and they're essentially a write off. They're huge. They're awful to deal with. Kendra, I would love to know, were there mistakes or denials that surprised you once you dug into the data that maybe were a little bit more transparent than maybe before?
Kendra: I guess how I would answer that is we were able to find them faster because we, like we said earlier, we weren't looking at those clean claims. We were quickly easy to see. Like one scenario that came to mind was Nebraska, Medicaid, actually, I know you're sitting down, offered to pay another code. Hey, if we can get any more reimbursement from Medicaid, we wanna get it right.
And we were able to identify right away one of the Medicaid payers in the state does not want the therapy modifier.
Justin: The
Kendra: other two do, but this one doesn't. So we're able to work with Prompt to create a custom rule just to strip that so we're not, otherwise, what our billing team was doing was removing it, rebilling it, and you have to wait another, 30 days.
And that seems. Silly when we know what the problem is. And so we have several scenarios like that where we, you identify why are we paying someone just to rebuild it when we know we can fix it right away. So we sometimes we can set up in the system like like Phil was saying with the EIM code.
You can set those up by payer if they're following the G or 3 0 2 8 3 or they want the 9 7 1 4. You can set that up. So it's telling your therapist when they're billing which code to use the pair changes their mind tomorrow. You can change it in the system right away tomorrow. Yeah. Yeah. So those claims go outright the first time.
But, and same with like that code that Medicaid was gonna start paying, we were able to set up that rule, have that modifier strip so the claim goes through clean. Nobody's having to retouch it, especially Medicaid pair, where the margins are so tight. Anyway, we don't need anyone else touching that claim again.
Josh: I think that's great to be able to identify those patterns within payers or even plan specific patterns that you can then action on and, make root cause changes to have them go out clean. I think that's a great thing too. One of the, I'll share one. We had a client that you know.
There's a payer back east that when you bill 9 7 1 4 oh and 9 7 5 3 oh together, whether you have the 59 modifier or not, they actually don't pay unless you send documentation, right? So it's oh, we didn't know that we weren't getting paid a bunch. Because we were doing this and no one ever told us.
So just enlightening them to that so that they can change or better operate so that now they're getting paid that full amount that they're supposed to be getting was a huge thing for them. And it was just so small to just be able to see that and then make that backend change of, or operational change to, to push that forward and get more revenue for them.
So yeah. That's great.
Kendra: That's a good point, Josh, on the CI edits, so prompting obviously has the normal quarterly updates in the system, but there are those payers out there that we won't name that want specific, they're following like an old CCI edit and we're able to identify those and set those up by the payer.
So then the therapist does get prompted and they don't have to remember to add those 50 nines. It tells them what to do. So those claims go through the first time. Same thing, we'd get the denial, throw on the 59 and rebuild it. Why do, why are we doing that? And so we're able to identify those a lot faster and get the claim hopeful.
Hopefully then it goes out clean, comes in clean and nobody's touching it again. That's the goal.
Justin: Yeah. And I think to that point, like I see a lot of questions and I know we're gonna answer a lot of them later on. But to kind of Kendra's discussion earlier with the auto posting rules and like how we best implement those.
I take a very similar approach when it comes to some of the automation. And rule building that you can do with the, either the CPT blocks and then also the modifier rules that you can set up at the address book level. And I see a couple questions on here about, different 59 modifiers and CCI edits and everything.
Is we put all of the P one and P two edits in there quarterly. Everything's updated for if you have the NCCI edit. Selected in the address book. But to Kendra's point, so many payers are usually a quarter or two behind, or they'll hold onto some old ones, especially the private payers. You're able to set up those different rules using what we call like the trigger code.
So you know, if you bill this code with this code, append, this modifier on it. And an approach I take to adding those is using my, either the claim success report out of the reporting module, or the failed edits and rejections report as well. And I start tallying them up. Hey, I'm having the same thing.
Come back for this payer so many times. Is there a rule I can put in place? I take the highest volume first. And I see a question on here too. Someone said, what are the best reports to use? I can speak confidently, at least on the RCM side. I, some of them might be. Scheduling and stuff that's beyond me, but is I take the claim success report by process date and I try to run that every week.
And when I do that I catch the last week as well and then I organize it. I sort the Excel sheet by my highest volume denials and the highest payers. If I have the same denial coming in for the same payer at the top, chip away at three of those at a time. See if there's a rule you can put in place.
If there's coaching, you can do. Or just any kind of notification so you're not catching those. And to Kendra's point, just adding something to send it back out every time you're adding something, just to send it out, start asking why is this something that I can put a rule in place and prompt the therapist to do it on the first time.
If it's something that's maybe not natively available in prompt at the moment or your EMR. Can I do an EDI edit or a custom rule? Anything that just helps again, catch those faster and you're not catching them on the backend. Every time you get a denial and you resubmit it, you're pushing that out another 14, 20 days.
And so anything you can do faster on the front end is always gonna be better. And then the other one too is a lot of the issues do get caught in the billing module from what we call the exceptions or the rejection. So a soft failed edit, a clearinghouse rejection, anything like that. Or UHT loves the, what do they call those?
Smart edits. So you'll get those back and what I like to do is there's a failed edits. In rejection report and you can run that and do the same thing. What is your highest volume? Is it something you can work with your front desk on? Is it a benefit verification issue? If you take those highest volume ones and you work on making them not your highest volume, like you start noticing everything go down those are two reports.
I liked just on the back end to catch things that typically you can correct on the front end. And then on top of that, I think anyone like working in RCM, obviously using some form of an AR report and however you're tracking your actions is obviously very important too. Work your first touch denials and then start working your aging and.
Have a standard cadence to Kendra's point too, of working in the platform and seeing when you took your last action and like leaving a note on those. And you can use tags and there's a lot of other features there that let you know, Hey, this needs to be followed up on next, or this is still outstanding, is super important.
Kendra, what have you found to be the most useful when you're trying to catch those missed opportunities or just make sure things are being followed up in a timely manner?
Kendra: I agree with you on those reports, catching trends 'cause it's easy to catch the volume and then you can easily tell what's.
Legit weed those out and then get to the ones that aren't. But else the other big efficiency for us is, in our legacy system, to catch anything wonky like that, I would had to run tons of reports, stitch 'em together, really dig into it, and then pull up the claims. And it just was clunky, if you will, like this new code that came out for Medicaid, for example, I gave it a couple weeks and I'm like, is it paying?
I didn't even have to go run a report, within billing, I can put that code in. And hit. Filter or whatever. I can't even think what the button is right now. And it would brought, and then I could, I have all these claim examples right here at my fingertips to see is it paying And that's when we are quickly able to identify that one doesn't want the therapy modifier, but I didn't have to do a bunch of research and stitch reports together.
It was just really easy to identify. Or if a partner wants to know, Hey, what's a certain payer paying on a specific code? Or are they paying on a specific code? You can run those filters right within the billing. Boom, we've got all the claims you need to dig into. So that's made it way more efficient and easier to identify issues that we can control potentially, or provide feedback to the payers whether they want to listen or not, but
Justin: fight the good fight.
Kendra: Yeah, exactly.
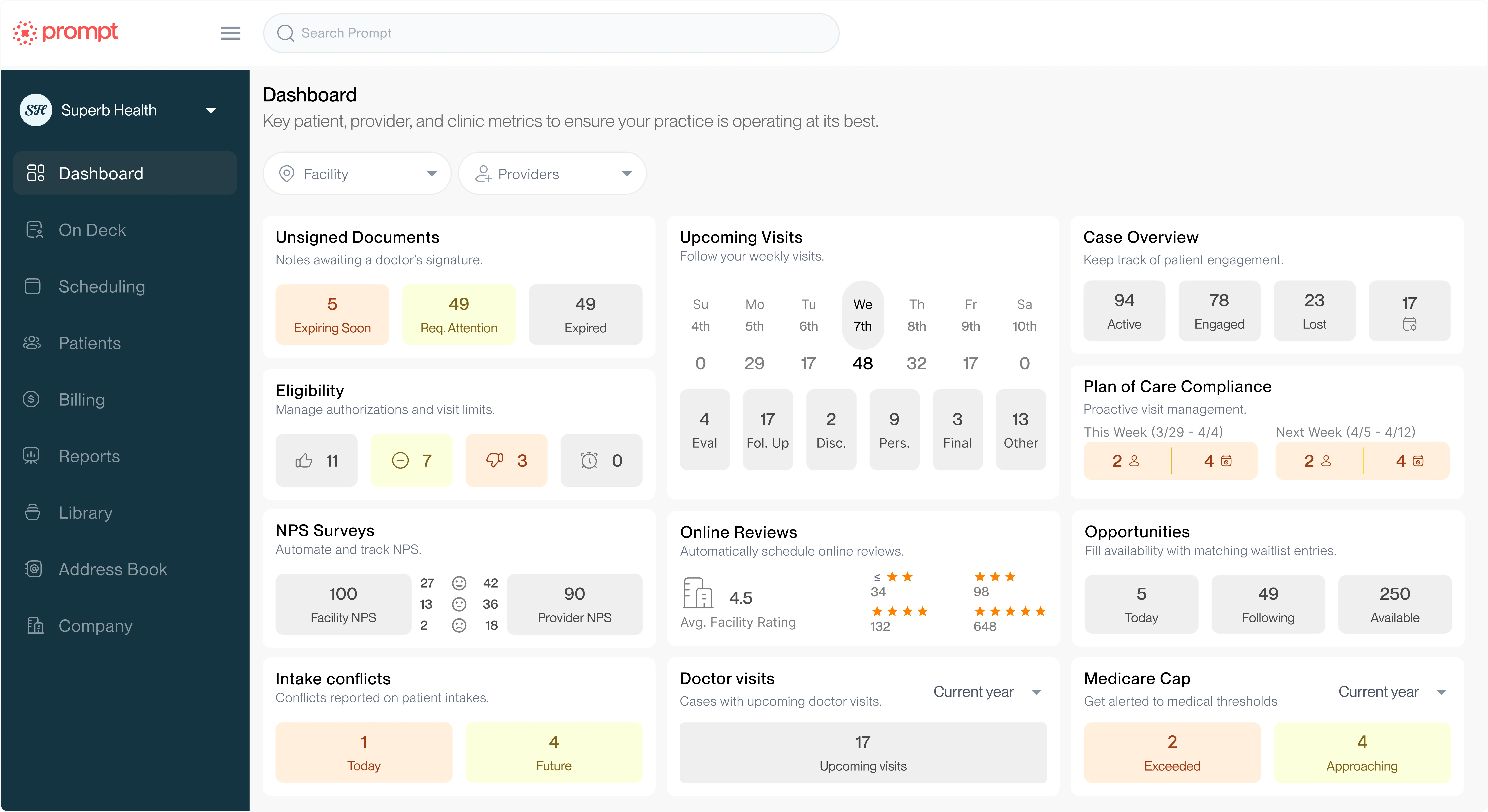
Josh: I think that's great that you bring that up, Kendrick, because that's a. That's a great way to, to look at things is like there's levels to it, right? Like you can look within the billing, but then you can look at the dashboards within the reporting and then if those still don't make sense or you want to get even more granular with it, there are the Excel reports, right?
So it's it's very efficient, as in to what level can you utilize to take actions on or see what's going on. And a lot of times when I talk with clients, we build out their KPI stuff and I'm like, if you come to this dashboard and you're within or below, like for denial rate, let's say you're hitting your KPI or you're below it, don't even bother digging in for there's no point to digging in further.
And maybe once a month, maybe once a quarter. But certainly don't be doing it every day or every week or anything like that. Again, you stop chasing ghosts, right? Because you can identify things, do that waste time. Phil, I'd love to hear what kind of reports you pull or you rely on as a practice owner and what you like to look at.
Phil: I'm still mudding through a lot of the case reports in ar, so I've been working with my RCM. Contact and she's been helping me get the data that I need for my KPIs and through our business intelligence data. So I have leaned on her more heavily than not, and then she's gonna hold my hand and get me onto running those without training wheels here relatively soon.
But I'm still training wheels.
Justin: I would say Kendra, that brings up a good question too, as we talk about third party billing. I saw someone in the chat also had asked where you get the big fancy financial reporting. So I think there's one piece of it. Obviously there's a lot of native reporting and prompt that anyone can pull that's a user and has permissions.
But then also as like third party billers, like I think it's a lot of times our job too at the end of the month or the end of our like, invoicing period, right? To provide analytics of one. What we provided service wise. But then also help, like I look at it as a partnership, identifying trends of not everything can RCM magically fix.
That's a, it's a partnership of, maybe there if you're not having, benefits, often verification, all that kind of stuff. If you're not having that happen. On the front end or with your RCM partner, whatever's happening, there's a downstream effect. And so I look at those like at the end of every month, our RCM service, and a lot of them do this it's like a monthly business review or kind of a reporting session where I like to point out, Hey, here's the things that we collected on.
Here's what went well, here's areas of opportunity, and then also the mysterious write-offs. I always like to present those too, of Hey, this is what's. Sitting there that might not be collectible and here's why. One thing I think as like billing partners is not to be like a finger pointer and it's a partnership.
We make money off of each other as well. So it's if you're doing better, I'm doing better. And I like to provide as much like clarity and transparency into that. And. As like Powerhouse is a partner with Prompt two. I think it's just what are approaches you take with your partners to provide the transparency that open communication?
Because so many people have been burned by bad partners in the past, I feel like sometimes we do extra handholding to bring 'em back.
Kendra: I agree with that 100% Justin. And that's one thing we just, we tell all of our clients, we're completely transparent. You can see what we see, make sure we're doing our job, we're trying to do our job the best we can.
But whatever we can see, you can also see nothing's hidden. You can pull all the reports we can pull, but then monthly going over. What are the top denials for the month? What are we seeing in that market? Sometimes it's market driven. There's some payer issues that are happening and we know about it.
Or maybe there's some potential education on, or discussion on coding and billing and how the therapists are billing some things and, hey, you're potentially leaving revenue on the table 'cause you're not billing enough to capture what they're allowing. Or, Hey, do you wanna look at this contract? It's paying lower than this other payer and here's why.
Maybe we could dig into those things a little bit further. So it just depends on, what we're what's coming through for the month, but having those open discussions, I think that's the key. Like you were saying, like just being open and saying, here's what we're seeing. Or maybe here's something we could use your help from your front desk staff, we're seeing these couple trends, maybe did you have somebody new start? Could we, talk to them, whatever it may be. And that's really helped. I feel like keep the, keep everything open and moving in the right direction.
Justin: I agree. How many times do people wanna hold your partner accountable?
Like they wanna say, Hey follow up on these in a certain cadence, which is absolutely valid, but then it's also, there's times we need help, whether it's from the clinician or the front desk. And I always joke, I'm like, you hold us accountable and we'll hold you accountable too. And if we're sending something and we need help with it or we need more information we're only as good as what we're getting.
And so sometimes it's just like to having that open discussion, sometimes they're uncomfortable, but I always like word, it is like, where. Your business partner and we wanna get these pages as badly as you do and Right. If there's something, extend, like holding us up for too long or anything.
I wanna have those conversations and have a, that clear work stream. And I think that's something too that I've noticed with a lot of other people oh, this would get hidden in this kind of task or this area. And just like pointing those out too. 'cause sometimes you don't know what you don't know, so it's just having a conversation and making sure that's available is definitely a huge piece.
Which brings me to one other kind of big question. With everyone is, this is the first platform I've worked in where not only internally communicating, can you do it through tasking, but then there's also the at tagging function which I think for RCM is huge. Have you utilized that feature a lot, Kendra?
And have you, what have you found with that?
Kendra: Oh yeah. I'm looking at the number of chats I have and yes, my team uses it. We, it is very I really like it because you're able to see on a claim instead of things getting lost in emails. You never know if somebody's sick or not there that day or on vacation.
It's a lot to keep track of. And so if it's all right there within the claim, whoever's working that claim or opens it up to take a patient phone call is able to see exactly what's happening. So that's been very helpful to have it all right in there. And I don't think we talked about this yet either, but going into something you just said about we're a partnership.
Even like thinking so Phil's the therapist, Hey Phil, I need your help on this claim. The claim isn't just sitting in my bucket and I. Emailing him anymore. That's how it was in the legacy system and that made it difficult. So then I constantly am following up. Did I hear from Phil? Do I, did he email me back and now I need to handle it.
Where's it at? Now it's, I send it to Phil, it's in his bucket. So the claim isn't in multiple, buckets, if you will. If I need the PT to look at it, I send it to them and it's in their bucket to fix, or it's in the billing bucket. And so that's made it a lot more clear. Truly who's, responsible for the next step potentially.
So that's been I just another efficiency gain for us.
Justin: Just send it back. I'm like, Hey, get it back to you. You go, Phil Hey, I finished my notes. Let me go check my email and the tasking platform and everything. It's, I can't do what I need until the next thing is done. Get it outta here.
And so it just to be able to send back right in the platform.
Josh: Yeah, that allows for that partnership a lot easier, right? Is 'cause it's clear taskings to who's responsible for what. And there really isn't that finger pointing. It's just oh all right, I'm up. I need to do this and send it back.
So I think that's great. I think that's one of the best things. Some, just practice owners. I do own clinics and I think one of the best things that a practice owner could ask, the RCM, if they're utilizing prompt or just anywhere is you're seeing this trend, what can we do operationally to stop that from happening, right?
But in order to have that, you need that communication or that transparency from your third party builder or the platform you're on in order to even ask those questions. Being able to ask those questions is a huge thing and have it guide your processes so you can stop those denials.
Like Justin said, RCM can't magically stop some of that stuff. It gets, it goes out that way.
Justin: Then another question. I think this is a great one for Phil, just so Phil's obviously newer on the prompt software, but he also does use the prompt R CM service as well. He was also one of our first customers that is like kind of trialing and piloting our. Benefit verification and authorization platform.
I guess Phil, from that process, I know we were very open in the beginning with you as well, saying that was, you were one of the first ones with that. Do you have any kind of experiences with that? Whether it's collaboration or feedback and like I know you've plugged your support personal already a couple times and that you have great communication, but I guess just how has that looked different than I guess, your prior service too?
Phil: And I think you guys were op, very open about it, but we were very open about the want to if you guys are willing to do this, we are already spending resources time. Don't let that go to waste. If there's someone who could pilot it, we're already probably staffed to help with that.
The amount of hours that my business partner or my myself spent two clinicians, like if we can come and help and there's some bumps. We live in bumps with legacy, so we're very willing to jump on that ride. It's again the concept of communication and collaboration without finger pointing.
I'm probably more email heavy with this than I need to be. Because of the trust and getting just into the system, especially with some of the ones where retro odds are less favorable with regard to backdating and things. So I probably haven't gotten the efficiency there yet, but the communication is.
Has been wonderful. The carryover has been wonderful. No reason to lack of trust, and I think it's nice. I have one point of contact which is, has been great. And again, she's come through every time I'm told when I need to do things also, which I was this morning with regard to one of our payers and it's communication and teamwork, which is solid, and that's the goal.
Justin: Kendra, how do you notice on your customers and everything like one would go and then also with just powerhouse of like how benefits and verification and everything are and authorizations too are tracked. Do you notice that a lot of times being like a centralized team or a clinic like.
Front desk handling it. I know that's like an issue that I feel like everyone struggles with because the rules are always changing and the payer are always changing. And I've seen a lot of people in the chat like EBV, like electronic, ver like benefit verification's. Amazing. But there's also times it doesn't work the best.
It's only as good as the information returned by the payer. And I see people talking about P Verify and. I can speak the RR Sam company definitely uses P Verify, but there's, the information's only as good as what the payer provides back. So I know internally we've created a matrix of, hey, these ones we've been able to process and check and like we, we validated that these ones are good.
Some of the other ones, maybe we do need to do a phone call or we need to do a portal, kind of investigation into how has your team experienced that and worked through that?
Kendra: Yeah I feel it's definitely been a win for us from comparing to our, like our legacy systems where our auth team was tracking it in Excel files, and then they're sick.
Okay, where's the Excel file? How can someone jump in? Now it's all right here within Impro, the claim doesn't leave the door if there's no auth on it. There's no. Letting claims slip through as long as we've got the payer setting set up correctly, so that's obviously a win.
And we do, as going back to your staffing question, it's more of a centralized team is typically what we see. 'cause you, with 19 clinics, not every 19, not every clinic's doing their own. We have a more centralized, so one person might be handling four of the clinics and then because they're a smaller team, they're able to.
Keep up with the changes. 'cause you're right, the payers are changing the off processes all the time and it's hard to keep track and so that makes it a little bit easier. As far as our powerhouse clients, a lot of 'em are not as big as go. And so they have usually like one person doing 'em at their clinics.
And then a lot of it is like we just, we share information back and forth with our clients as we learn things in those states because. It's hidden. The payers hide that information or we, if it's something we can code on the payer and prompt to make it easier for them, we will. So that's helped a lot.
And then, like you guys have I don't know what else to call it, but thumbs, red thumb, yellow thumb. That's helped really know where to start. I feel, and there's filters within that. I think it's, is it on the dashboard? I don't use it every day. Yeah.
Dashboard, so it's easy. Yeah. The dashboard. So if I am just working work comp, for example, I can go into that dashboard, go look at my thumbs, but filter it just for work comp and then I'm gonna start with the red. Okay. Have I missed any, through my other channels or which ones are out of us And they're still coming.
Okay. I need to. Ping the therapist to ask if they should be discharged. Are they still coming? Do I need to get another auth? Whatever, handle those. Then move back to the yellow and then, so it's helped really, I feel like the off team understand or help them prioritize a little bit easier also.
Justin: I do the little thing when you open up the thumb and it goes to visit calculation at the bottom and it will literally tell you like what ones are covered and what ones aren't. So like when you're trying to go back and reassociate or figure out what was maybe missed it's very clear I used to have to download different ledgers and like review and like count to each visit.
Yes. Yeah. And so it's nice where you can just pull it up and you're just like, these ones are good, these ones I still need to work on. And prioritizing is a huge,
Kendra: and we used to talk, but building off that Justin, sorry, I didn't mean to interrupt you, but like with the thera we used to send manual spreadsheets to the therapist.
Hey Phil, here's your patients that are about out of office, and Hopey opens it right in the same day. And now they have what is it called for the the day DA Daily rundown.
Justin: Yeah, the rundown.
Kendra: Daily rundown. So you know, it shows you right there, here's who's coming in, here's who's about out of auths, whose needs an auth.
Okay, I haven't heard from my auth team, or it's pending, or maybe I don't wanna see this patient today. Whatever it is. So that's helped a lot I think just with communication back and forth 'cause. If things get lost in email, it just doesn't work. It's just not efficient. So you wanna
Justin: be like one centralized place.
That's one of my biggest things with even running multiple like RCM teams is I don't want someone to have to log in the computer, open their 10 other spreadsheets, their other thing over here, and like they spend 15 minutes prepping to start work. Log into the cloud-based EMR and ideally most of it's right there and like you're not having to, do too much other things.
And also, like what happens in your computer reboots and you have to go find all your files again. It's you're paying for this cloud-based EMR and I think that's something is you just wanna go in there and dynamically work as much as possible. And it's secure. And again, just sending things and not having to go check your five other emails and tasking and spreadsheets and your shared sheets and everything like that is just a huge piece for efficiency.
Social security is a big part of it too. Yeah,
Kendra: that's a great, and Justin, sorry, go ahead Josh. Go ahead
Justin: Kendra.
Josh: I just wanna say that's a great call out by you both that for everybody on this call, I just wanna reiterate, if your clinicians aren't using the daily rundown, you may want them to look into that because that is the central hub for each patient and there is a ton of information there that you can get.
So again just wanted to call that out real quick. Kendra, sorry to interrupt.
Kendra: No, thank you. Yeah, no, I was just gonna build off Justin saying, you know how you have to log into all these systems. I don't think we talked about this yet, but from the RCM side, you used to have to go into the clearinghouse work rejections, and then maybe even look up remit information.
All of that now is housed right within prompt. So you don't even have to log into the clearing house. You're working the rejections, whether it's a. Prompt rejection, a clearinghouse, rejection's all right there within prompt. And then also when the remits come back and they return it as any, anyone, any billers out there.
CO 16, what the hecks that mean? Yeah,
Justin: could be a million different
Kendra: Thanks for the information, if they do return a remark, that also comes through prompt. Yes. And so before, in our legacy systems, we'd have to go pull the remit from the portals or from the clearinghouse. Now we can just hit that.
Beautiful remark button right there on the claim and missing documentation or whatever it is, actually tells you what the problem is versus a generic code.
Josh: Yeah, those card codes are great, but they don't always tell the whole story. You need those
Justin: in there, Medicare, get your remark codes in there.
And then another thing I think too, that was like going back to not needing to go in the clearing house and one do rejections and stuff, but PBS is another big one. And having that surface, like in the remit where you don't have to go find the little print at the bottom of it and figure out what it means.
Just again, bringing that to people's attention faster and ideally, again, not logging into multiple systems to find those is super helpful and just more efficient in general.
Josh: Yeah. Which you can explain to them too, right? Like why their paid amount is different than the check amount. Yeah, exactly.
Right.
Justin: Where are we borrowing to pay this next thing from and that
Josh: Yeah, exactly.
Justin: Oh, go
ahead Kendra.
Kendra: I was just gonna say the only thing constant has changed, and I feel like that's one thing and Phil's probably seen it a little bit, even just being with PROMPT for the 120 days. But we've been with Prompt for, a little over a year.
There's constant updates and PBS to Justin's point is one of them that was not here, 15 months ago, and now it's right here at her fingertips. Just. Those little things are big things actually in the RCM world, and I know there's been a lot in the therapist side too.
Justin: Yeah, and that's, that's just to plug for everyone here, that's a prompt user too, like the, I would say the next.
What is it really? Four releases pretty much through the end of the year are heavy on the RCM front. And so I've seen a lot of questions and we'll go through some of the q and as too and go through the chat in this last 10 minutes. But a lot of the things that I would say are big hitters.
We have a denial queue coming out, which is, I know everyone's very excited for. Just like increased, I would say visibility and AR in the actual billing modules. Self. We just made a lot of changes too to the AR ledger and like the way things calculate with the negative AR and not making over adjustments and one of the things I see some people also mentioning are just like, Hey, like how do I talk to someone that, can go through some of this stuff with me?
It doesn't even have to be Kendra, myself, or Josh. Really any of our billing success managers here at Prompt. And if you're a client that's been with us for a while too, and you maybe have fallen out of touch or not have like daily, or not daily more regular cadences you can reach out to either support and just ask, Hey, who's my BSM or billing Success manager?
Everyone here is trained to have these conversations and we also. You can reach out to support if there's not a problem. And I think like Kendra, we're on a pretty regular cadence. Like we can just go through things and talk about the new updates, see if there's like opportunities.
That's one thing I love to do with clients is just go in there and just look at things and I like point out, Hey, have we looked at this? Area for a while or, Hey, have you started using this? And so definitely reach out to the support email if you have don't know who your billing success manager is.
Everyone that's a prompt client has one, and they're more than happy to hop on a call again with nothing wrong. Just have the conversation, go through some of the updates and just make sure you're utilizing everything. And that being said, too, these next four updates that are coming out, the releases are quite large on the RCM front.
Please reach out and see how it like, fits into your workflow the best. Some of them are settings you have to turn on. Some of them are things you might just have to adopt over time. I always like to have those conversations, but maybe it's not day one. You're gonna start, changing your workflow a hundred percent, but how can you slowly integrate it without disrupting anything is always a really important piece.
There's one question in the QA I just wanna answer and it's about, pretty much CPT code. So whether someone's using a G Code or if they're using a normal, standard CPT code, there's a couple things you can do there. It says one, one of the questions is a way to just universally put it across all payers.
From a an EMR compliance standpoint, we're not able to like, suggest too many things automatically just depending on the individual payers in the regions. But there is one thing we can do is one, reach out to your billing success manager. We have access to a lot of data so we can tell you regionally and geographically what we're seeing in those areas or with those different payer codes.
And then the other thing is we're happy to help. Set those rules up in your address book too. And just talk through it. If you're noticing this payer doesn't cover the standard CPT code, let's put a block in. Or is it one that we need to put the G code in? We can do that as well. And then last but not least, I feel like it always comes up is what happens when the primary payer covers one and the secondary is a different, we do have EDI edits that we can help you set up there too.
So those. Crossover or crosswalk if needed. So again, just reach out to your billing success team and we're always happy to answer those questions or help you with any of those kind of automation needs. David was the one that asked that question, and I have just another kind of piece. Roadmap wise, one thing we're working on with our acquisition of Prediction Health is just more AI insights.
Whether those are just recommendations or trends that we're catching. So in the near future, we're hoping to have more things that kind of come out and say, would you like to these suggested rules? We're like, see what people are using in that, with that payer. And again, we're not gonna just auto set those for you because we want you to have control.
But at the same time, we wanna be able to. Give you suggestions on what other people have learned or what we've seen throughout the product. So we're trying to help increase that visibility as much as possible.
Josh: Yeah, I think that's a great segment into talking just about how you can partner with experts here at prompt to help you on any level that you're at.
Because as Justin was saying, those bsms can certainly answer to things. If they can't, they'll know where to point you. Whether that be RCM if you need it or the coaching division. We're stand standing up if you need a little more white glove from there. Or even our preferred partners, which we have one on the call with us right now, if we, if you need RCM with.
With Kendra or something like that. We always wanna point you to the right expert to partner with, and we want to be partners in your success and that's our mission. Like Justin said, just reach out to support. They'll know where to direct you for sure. If they can't handle it themselves, which.
The majority of the time they will be able to.
Justin: And then you'll notice a poll just popped up on everyone's screen as well. If you answer any of those questions, we'll follow up with you guys. If you wanna talk to anyone on the panelist list or learn about just anything we put the contact information in the chat and then if you were to select any of that on the poll, we will distribute that list and everyone can reach out afterwards as well.
Awesome, Kendra, Phil, any kind of closing remarks you guys have for the team? It's been a team. I appreciate that.
Kendra: Yes. Thanks for including us.
Justin: Absolutely amazing. Thank you everyone. And if you guys find this like to be, this is our first time doing more of a just an industry kind of talk especially on the RCM front.
So if you guys have feedback or anything, feel free to put it in the chat. And we're happy to continue these conversations. I think it's something that everyone in the space gets into it to help patients. And RCM is. As fortunate or unfortunate is the backbone of making sure we're getting paid and able to maintain this.
And so I think it's always something that there's so many just questions on. And it's like we said, the only constant thing in RCM is unfortunately change. So we've gotta keep up with it and keep these conversations going and working together to keep fighting the good fight. Amazing. Thank you everyone, and we will talk to you all soon.
Thank you guys.
Bye.
Bye guys. See?