See Prompt in action!
For those of us in the physical therapy field, understanding the nuances of coding can feel a bit like solving a Rubik’s cube. The complex world of coding is made even more complicated by different rules for different insurance types, all with their own jargon.
Today, let's unravel two crucial AMA billing rules: the Total Minute Rule and the AMA Rule.
Often dubbed the Medicare "8-min Rule," the Total Minute Rule is one of the key methodologies employed by Medicare and other federal payers.
Conversely, commercial insurance providers usually lean towards the AMA Rule, also known as the Substantial Portion Methodology (SPM) or Rule of 8s.
However, in the throes of a bustling clinic, we sometimes find it difficult to distinguish between these two methodologies and make sure all therapists within our organization understand the rules and are using them correctly.
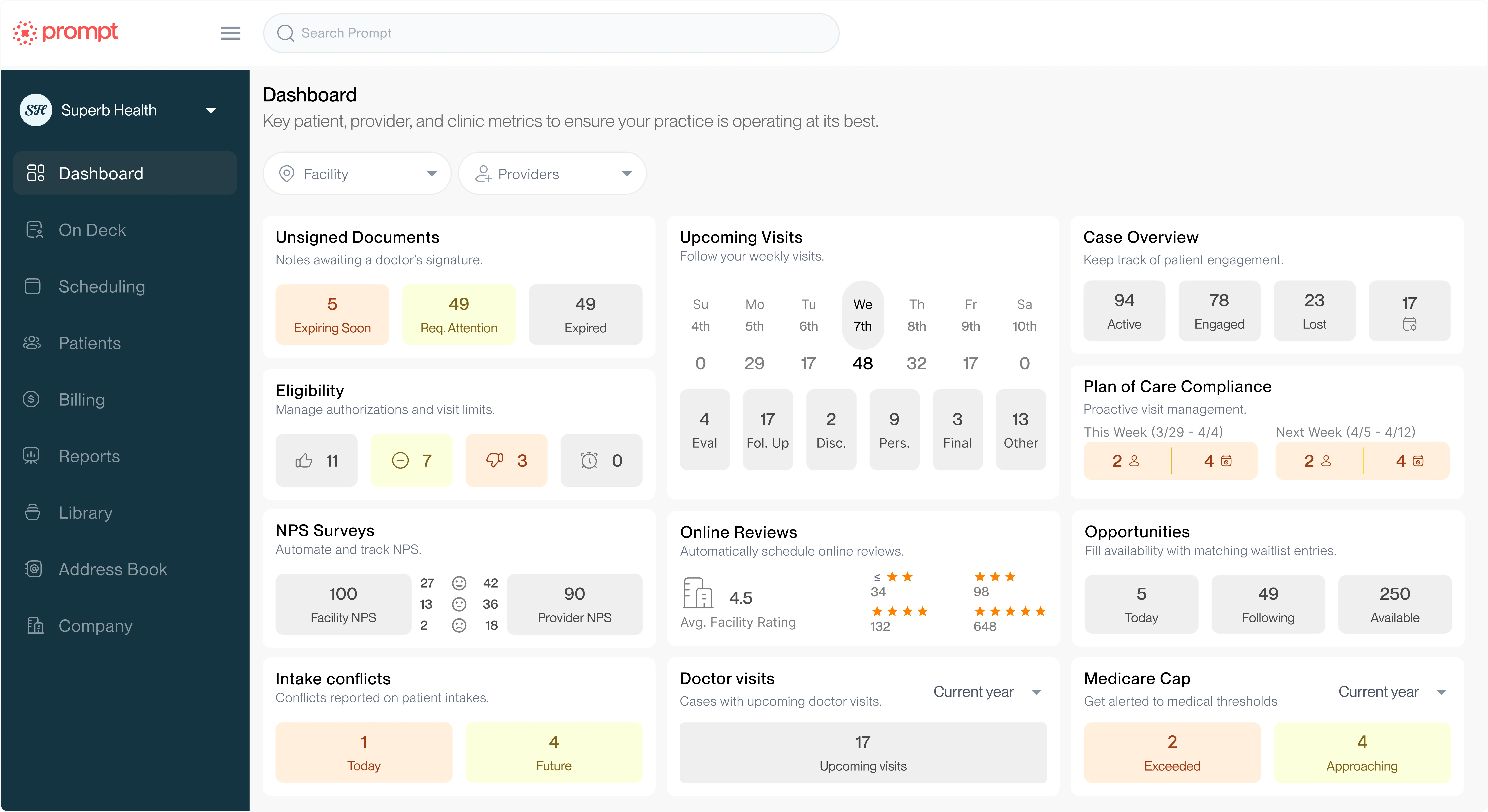
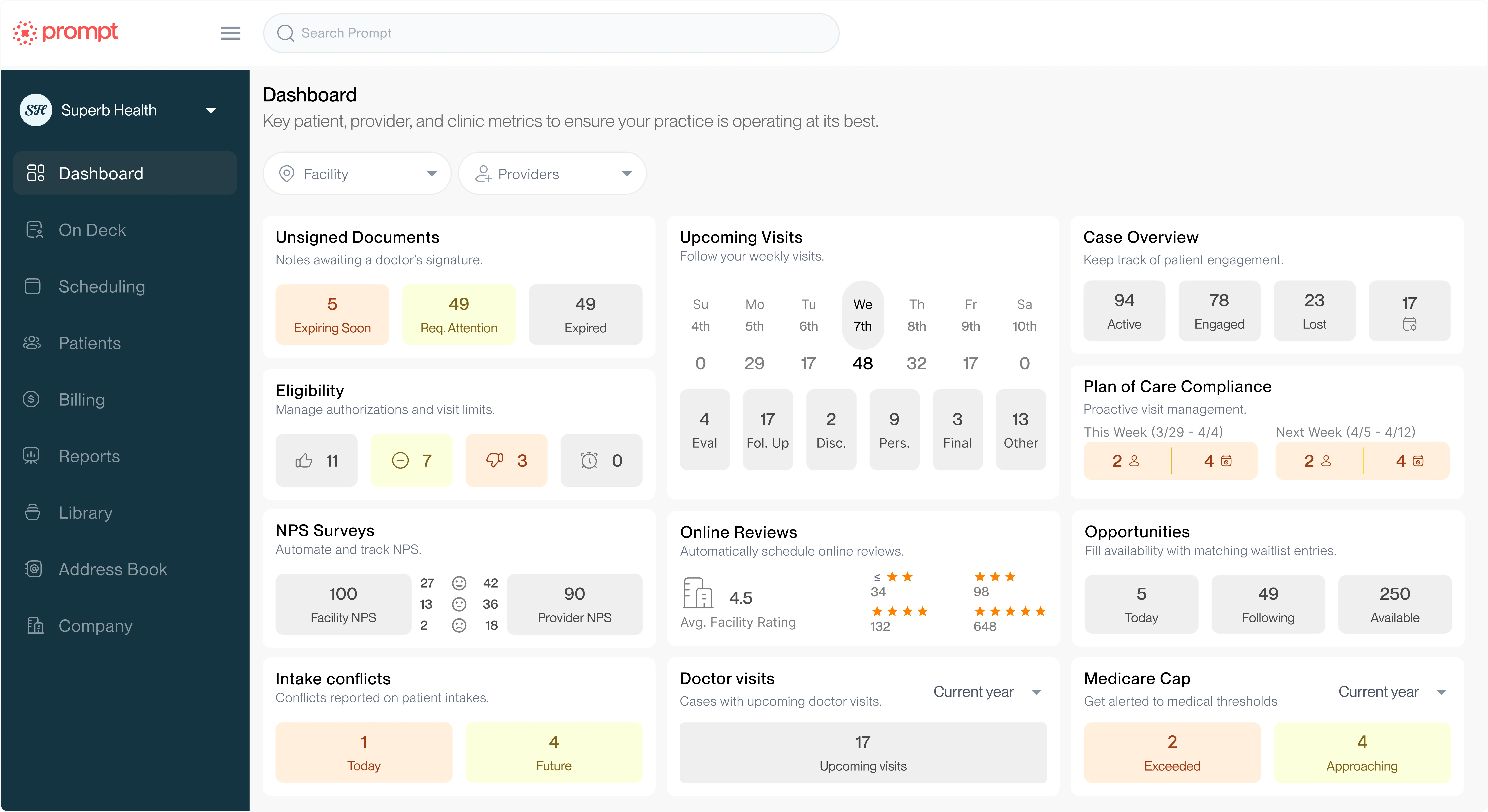
This is where Prompt's AI tools (formerly PredictionHealth) steps in, offering a clear, user-friendly way to determine if your therapists understand and apply the appropriate coding rules.
The Coding Efficiency feature within the Insight platform allows practice groups to easily track how therapists are coding and helps to identify where there may be opportunities to more efficiently code visits to ensure no units are being left uncaptured.
The Total Minute Rule calls for billing based on the overall time spent with the patient, regardless of the various CPT codes that could be involved. We simply total the minutes to calculate the number of units we can bill. Here's a quick breakdown:
The AMA Rule, on the other hand, hinges on the time spent on each unique CPT code rather than the total time with the patient. For each unique CPT code, 8-22 minutes equates to one unit, 23-37 minutes equates to two units, etc. This incentivizes therapists to bill multiple unique codes, each clocking at least 8 minutes.
To clarify the difference between these two rules, let's dive into a few scenarios:
Let's imagine a scenario where a therapist bills 10 minutes of Therapeutic Activity and 8 minutes of Manual therapy, totaling 18 minutes for that appointment.
Under the Total Minute Rule, the total appointment (the full 18 minuntes) fits in the 8-22 minute range, so it is billed at 1 unit.
Under AMA or 8 Minute Rule, there are 2 different codes that fall within the 8-22 min range, so you would charge 1 unit for each code, totaling 2 units for that appointment.
In another scenario, a therapist might want to bill 6 minutes of Therapeutic Activity, 6 minutes of Therapeutic Exercise, and 6 minutes of Manual Therapy. The total appointment is still 18 minutes, but it would be billed differently.
Under Total Minute Rule, 18 minutes fits in the 8-22 minute range, so it is billed at 1 unit.
Using AMA Rule, however, since none of the CPT codes were greater or equal to 8 minutes, 0 units would be billed.
For appointments longer than 18 minutes, the same rules apply. If a therapist wants to bill 10 minutes of Therapeutic Exercise, 10 minutes of Manual Therapy, and 10 minutes of Neuro Re-education, the total time of the appointment would be 30 minutes.
Under Total Minute Rule, 30 min fits in the 23-37 minute range, so it would be billed at 2 units.
Under AMA Rule, there are 3 different codes that fall within the 8-22 min range so you will charge 1 unit for each code, or 3 total units.
The previous examples have all used nice round numbers, but that isn't always how things play out in the clinic. In a situation where a therapist bills 30 minutes of Therapeutic Activity, 4 minutes of Therapeutic Exercise, and 7 minutes of Manual Therapy, the appointment comes in at 41 minutes.
Under Total Minute Rule, 41 minutes fits in the 38-52 min range so it is billed at 3 units.
But under AMA Rule,Therapeutic Exercise and Manual Therapy did not fall within the minimum 8-22 minute range, so you would not charge any units for those 2 codes. You would charge 2 units for the code containing 30 minutes (Therapeutic Activity).
We've broken out how many units each of these imaginary appointments would bill under both rules, but in reality, you wouldn't bill one appointment under both rules.
Medicare and some other federal payers like Tricare often use the 8 Minute Rule, while commercial insurers often use the AMA Rule.
But, each insurance payer will use a different billing methodology, which means when in doubt, it's always best to ask each insurer directly.
The differences between these two rules can be overwhelming, but it is important to understand the distinction, as they directly affect how much revenue your team captures for the care you’re already providing.
Knowing when to apply each rule ensures your documentation aligns with payer expectations, protects your compliance, and prevents underbilling that quietly chips away at margins over time.
But mastering these nuances manually is tough, especially when you’re balancing patient care, complex coding rules, and ever-shifting regulations. That’s where smarter technology can help.
Prompt's AI-powered auditing and documentation tools automatically identify how rules like the AMA methodology should apply, highlight missed billing opportunities, and give your team the confidence that every note tells the full, billable story of your care.
Book a demo today to see how this tool can help your team save time, ensure compliance, and capture the revenue you’ve earned.
Help your practice grow
From intake to insights, Prompt is the all-in-one platform you need