See Prompt in action!
SOAP notes and CPT codes are essential components of rehabilitation therapy, playing critical roles in patient care, ensuring documentation quality, promoting compliance, and facilitating reimbursement.
This guide provides rehab therapists with a comprehensive understanding of how to write effective Daily SOAP notes and accurately select CPT codes.
SOAP stands for Subjective, Objective, Assessment, and Plan. It provides a structured framework for documenting patient interactions, ensuring consistency, clarity, and continuity of care.
Example:
Patient reported feeling looser in the shoulder following the exercises and manual therapy completed during the last session. Expressed increased confidence in performing exercises independently at home, but described slight fatigue post-exercise. Patient reports continuing to have the most difficulty with overhead reaching. Current Pain level = 6/10.
Example:
Measured active range of motion in the right shoulder:
Passive range of motion is limited by pain at end ranges.
Interventions performed:
Example:
Patient demonstrates improved shoulder stability in the overhead position with continued progression in exercises. There is a reduced onset of pain in the right pectoral muscle during single-arm chest flys at 10 lbs (cable column) with adjusted angle of pull; however, patient continues to exhibit rapid onset of muscular fatigue, indicating ongoing weakness.
Example:
Continue progressive shoulder strengthening program focusing on rotator cuff exercises and scapular stabilization techniques during bi-weekly therapy sessions for the next four weeks. Addition of Glenohumeral joint mobilization next visit.
Accurate SOAP notes are a cornerstone of effective clinical practice, impacting everything from the quality of care to the financial health of a practice.
While they may often feel like a time-consuming burden for busy clinicians, these structured notes serve a critical purpose. They provide a clear, standardized method for documenting a patient’s progress, guiding clinical decision-making, and facilitating communication among providers.
Additionally, SOAP notes play a pivotal role in justifying medical necessity and ensuring timely, accurate reimbursement from insurance payers.
Without thorough and precise documentation, clinicians risk compromising both patient outcomes and compliance with regulatory standards.
In short, accurate SOAP notes are essential tools in delivering high-quality, goal-oriented care.
Accurate SOAP notes are essential for maintaining clinical quality by providing a comprehensive record of the patient's condition, treatment plan, and progress.
They serve as a roadmap for delivering consistent and effective patient care by documenting the patient's history, current status, and response to interventions.
SOAP notes facilitate seamless information exchange among care providers, ensuring continuity of care and promoting interdisciplinary collaboration.
Clear and detailed documentation enables healthcare professionals to understand the patient's needs, track changes in their condition, and make informed decisions about their care.
Accurate SOAP notes support legal and ethical practice guidelines by documenting the rationale behind treatment decisions, demonstrating adherence to professional standards, and ensuring that care is provided in a safe and effective manner.
Compliance with documentation requirements is essential for protecting both the patient and the healthcare provider.
SOAP notes play a critical role in demonstrating medical necessity, which is essential for claims approval and reimbursement.
By clearly documenting the patient's symptoms, functional limitations, objective measurements, and treatment rationale, physical therapists can justify the need for services provided and ensure that claims are processed accurately and efficiently.
Accurate SOAP notes serve as a critical tool for clinical decision-making by providing a comprehensive overview of the patient's condition, progress, and response to treatment.
This information guides therapists in adjusting interventions, setting goals, and optimizing patient outcomes.
Well-documented SOAP notes ensure continuity of care by enabling healthcare providers to understand the patient's history, treatment trajectory, and areas of improvement or concern.
This promotes consistent and coordinated care delivery across different settings and providers.
Accurate SOAP notes offer legal protection by documenting the rationale behind clinical decisions, interventions performed, and patient responses.
In the event of an audit, dispute, or legal inquiry, thorough documentation can serve as evidence of the quality and appropriateness of care provided.
SOAP notes play a vital role in quality improvement initiatives by facilitating data analysis, outcome measurement, and identification of best practices.
By reviewing and analyzing SOAP notes, clinics can identify trends, assess treatment efficacy, and implement evidence-based interventions for continuous quality enhancement.
Not all SOAP notes are created equal. There is a wide spectrum of quality that often depends on a clinician’s training, habits, experience, and writing style.
Some therapists may write overly brief notes that lack the necessary detail to support medical necessity, which can lead to claim denials, compliance concerns, or even audits.
On the other hand, the instinct to overdocument in an effort to “cover all the bases” can create its own set of problems. Excessively long notes may obscure key clinical points, waste valuable time, and even raise red flags during audits.
Striking the right balance is essential. SOAP notes should be clear, concise, and comprehensive, capturing the patient’s story and progress while also meeting clinical and regulatory requirements.
Below are some best practices that define a high-quality SOAP note and help ensure documentation that supports both care delivery and compliance.
Clearly documents the patient's narrative and clinical presentation: Include detailed information provided by the patient about their symptoms, concerns, and goals, as well as the therapist's observations during the evaluation.
Include precise, objective measurements:
Record specific data such as range of motion, strength, balance assessments, and other quantifiable metrics to track progress accurately.
Demonstrate clinical reasoning clearly in the assessment:
Interpret subjective and objective findings to formulate a clear diagnosis, prognosis, and treatment plan based on evidence-based practice and professional judgment.
Provide specific, actionable plans:
Outline detailed treatment strategies, goals, interventions, and patient education to guide the therapeutic process and promote optimal outcomes.
Be concise yet thorough, avoiding unnecessary details:
Present information in a structured and organized manner, focusing on relevant clinical information while avoiding extraneous or redundant content.
Use standardized medical terminology consistently:
Employ clear and precise language, follow industry-standard terminology, abbreviations, and formatting guidelines to ensure accuracy, clarity, and consistency in documentation.
Be patient-centered:
A high-quality SOAP note should reflect a patient-centered approach by incorporating the patient's goals, preferences, and values into the treatment plan.
This ensures that care is tailored to meet the individual needs and priorities of the patient.
Collaborate with the patient’s health team:
Effective SOAP notes promote interprofessional collaboration by clearly communicating the patient's status, treatment plan, and progress to other healthcare team members.
This fosters coordinated care, enhances communication, and supports a holistic approach to patient management.
Leverage evidence-based practice:
Good SOAP notes demonstrate adherence to evidence-based practice by integrating current research, clinical guidelines, and best practices into the assessment, diagnosis, and treatment planning process.
This ensures that interventions are grounded in the latest scientific evidence and tailored to the individual patient's needs.
Include patient education:
Including patient education in SOAP notes is essential for empowering patients to take an active role in their care. Providing clear instructions, explanations, and resources in the SOAP note can enhance patient understanding, compliance, and engagement in the treatment process.
Therapists take pride in delivering high-quality care and maintaining strong supporting documentation, but even the most experienced clinicians are susceptible to common errors in their SOAP notes.
These mistakes, whether due to time pressure, habit, or lack of awareness, can compromise note quality, increase compliance risks, and lead to unnecessary rework or payer pushback.
The good news is that many of these pitfalls are both predictable and avoidable.
By understanding the most frequent documentation missteps and learning how to correct or prevent them, therapists can improve the clarity and effectiveness of their notes, ensure compliance, and ultimately save time in their daily workflow.
Problem: Notes lack clarity or omit essential details. The provider documents vague clinical reasoning and justification.
Solution: Clearly and concisely describe patient complaints, objective findings, assessment rationale, and the specific treatment plan. Document why the patient needs care from a skilled and licensed provider.
Problem: Subjective opinions are mixed into objective findings.
Solution: Clearly separate subjective patient-reported data from objective measurements and observations. Tie the patient's objective measures to their decline in function.
Problem: Plans and goals are nonspecific and don’t tie back to patient function.
Solution: Provide clear, measurable, and achievable goals that tie objective measurements with patient function, along with detailed treatment strategies.
Problem: Use of different terms or uncommon abbreviations for similar conditions or treatments.
Solution: Standardize terminology throughout documentation to maintain clarity. Avoid the use of uncommon abbreviations.
Problem: Documentation fails to justify clinical decisions clearly. Provider does not document the ‘why’ behind the intervention, potentially leading to under or over-billing.
Solution: Always justify interventions according to the clinical intent behind the intervention. This will then help guide which CPT code should be selected.
Physical therapists often navigate a complex set of demands that can make high-quality documentation a challenge. Between delivering hands-on patient care, managing administrative tasks, and balancing responsibilities outside the clinic, documentation frequently takes a back seat or ends up squeezed into evenings and weekends.
These practical realities can lead to rushed or incomplete SOAP notes, increasing the risk of errors, denials, and compliance concerns.
Understanding the day-to-day challenges therapists face is key to finding solutions that support accurate, efficient documentation without compromising care or personal well-being.
High patient caseloads lead to time constraints:
Therapists managing large caseloads often struggle to keep up with compliant and on-time documentation.
This can lead to under-documentation and/or note-cloning (copy-forward).
Prioritizing patient care:
Therapists may prioritize direct patient interaction over documentation, leading the therapist to write the note hours/days later.
EMR challenges:
The documentation system may be time-consuming or poorly integrated into a clinical workflow. This can lead providers to double-document or errors.
Current Procedural Terminology (CPT) codes are numeric codes maintained by the American Medical Association (AMA) used to describe medical, surgical, and diagnostic services. Rehab therapists use these codes to bill payers for the services they provide.
CPT coding helps differentiate licensed and unlicensed practitioners, as well as skilled and unskilled care. These codes should tell a story in the progression of a patient throughout the plan of care.
There are different values held to each code, represented by how frequently it is utilized in the industry, as well as how much skill is required to perform certain interventions. CPT codes are reimbursed by payers at varying amounts based on the skill required.
Even with the best intentions, therapists can run into trouble when it comes to CPT coding. The complexity of coding rules, combined with time constraints, evolving payer policies, and subtle distinctions between codes, can lead to mistakes that impact reimbursement, trigger denials, or even raise compliance concerns.
Recognizing the most frequent coding pitfalls is the first step toward more accurate, efficient billing. Below are some of the most common CPT coding errors therapists make and how to avoid them.
Undercoding occurs when a therapist uses a code for a service that is less complex or time-consuming than what was actually performed, often to avoid scrutiny. This leads to lost revenue.
Overcoding, on the other hand, is when a code reflects a more intensive service than was provided, which can raise red flags with payers and trigger audits.
Timed codes (e.g., 97110 – Therapeutic Exercise) must reflect the exact amount of time spent on each billable unit, following the appropriate billing rule.
On the other hand, untimed codes (e.g., G0283 or 97014 – Electrical Stimulation, Unattended) should only be billed once per session, regardless of time spent.
Confusion on how to use both types properly leads to incorrect billing.
Therapists sometimes mistakenly bill for procedures that fall outside their licensed scope of practice in their state, especially with modalities or techniques that vary in regulation.
Therapists may use codes without documenting enough detail to support their use (e.g., lacking specific goals, patient response, or rationale for a manual therapy code).
This can result in denials during chart reviews or audits.
Some codes shouldn’t be billed together in the same session (e.g., billing multiple manual therapy techniques under different codes).
Using incompatible code pairs or billing two therapists for the same service (i.e., co-treatment errors) can cause issues.
Services performed by support staff (like PTAs or techs) may have different billing rules or restrictions under payer policies (especially Medicare).
Billing as if the licensed therapist provided the service directly is a common error.
97110 Therapeutic Exercise:
97112 Neuromuscular Re-education:
97140 Manual Therapy:
97535 Self-Care Management Training:
While CPT coding may seem overwhelming, there are a few ways you can make sure you're choosign the right code for your session:
While it’s essential for therapists to understand the fundamentals of high-quality SOAP notes, thorough documentation, and accurate CPT coding, these tasks can become overwhelming when layered onto the demands of daily patient care. That’s where AI-powered tools are making a meaningful impact.
By using ambient listening and intelligent dictation, AI scribing technology captures the patient-provider conversation in real time, generating fast, clean, and accurate clinical notes, all without interrupting the flow of care.
This technology is seeing rapid adoption among physical and occupational therapists thanks to its ability to improve documentation quality, increase coding accuracy, and reduce administrative burden.
The integration of AI scribing tools with EMR systems further enhances efficiency by automatically mapping structured note content into the appropriate sections of the chart.
As a result, therapists are experiencing measurable benefits, including:
Time savings:
Allows therapists to focus more on patient care and less on paperwork. AI scribing has been reported to reduce documentation time 50%-75%, allowing therapists better balance between and clinic and home life, which in turn is reducing burnout, turnover, overtime expense, and even improving productivity.
The fast sign-off times also aid in better billing practices and reduce accounts receivable (AR) aging.
Improved compliance:
When an AI model is trained on a specialty-specific compliance model, like physical and occupational therapy, it can generate consistent and detailed documentation aligned with clinical guidelines and payer requirements.
Organizations see as much as 30% improvement in compliance scores within the first month of implementing AI scribing because compliance guidelines are accounted for in the notes.
Enhanced accuracy:
Minimizes human errors and inconsistencies, improving CPT coding accuracy and reimbursement outcomes. A few AI scribing solutions in the market have built-in CPT coding functionality so therapists can understand in real-time whether or not they are selecting accurate codes.
In the case that they under or over-code an intervention, the AI can warn them and suggest a more appropriate code while still protecting the clinician’s judgement as the final say.
As with any clinical tool, AI should be used thoughtfully and responsibly. While AI scribing can significantly improve efficiency and documentation quality, it is not infallible.
Mistakes can occur, and clinical judgment must always take priority over automated suggestions. To ensure safe, effective use of AI in practice, therapists should follow these key guidelines:
Review and edit notes thoroughly
Always review AI-generated documentation to ensure it is accurate, complete, and clinically appropriate. The therapist is ultimately responsible for the content of each note, and oversight is essential to maintain quality and compliance.
Invest in training and systems familiarity
Understanding how the AI tool works, as wee as its strengths, limitations, and ideal use cases, empowers therapists to use it effectively without overreliance. Proper training also helps identify when manual adjustments or additional input are needed.
Prioritize data privacy and security
Choose AI solutions that meet all relevant regulatory standards, such as HIPAA, to safeguard patient information. Ensure your organization has clear protocols for data handling, storage, and access when using AI technology.
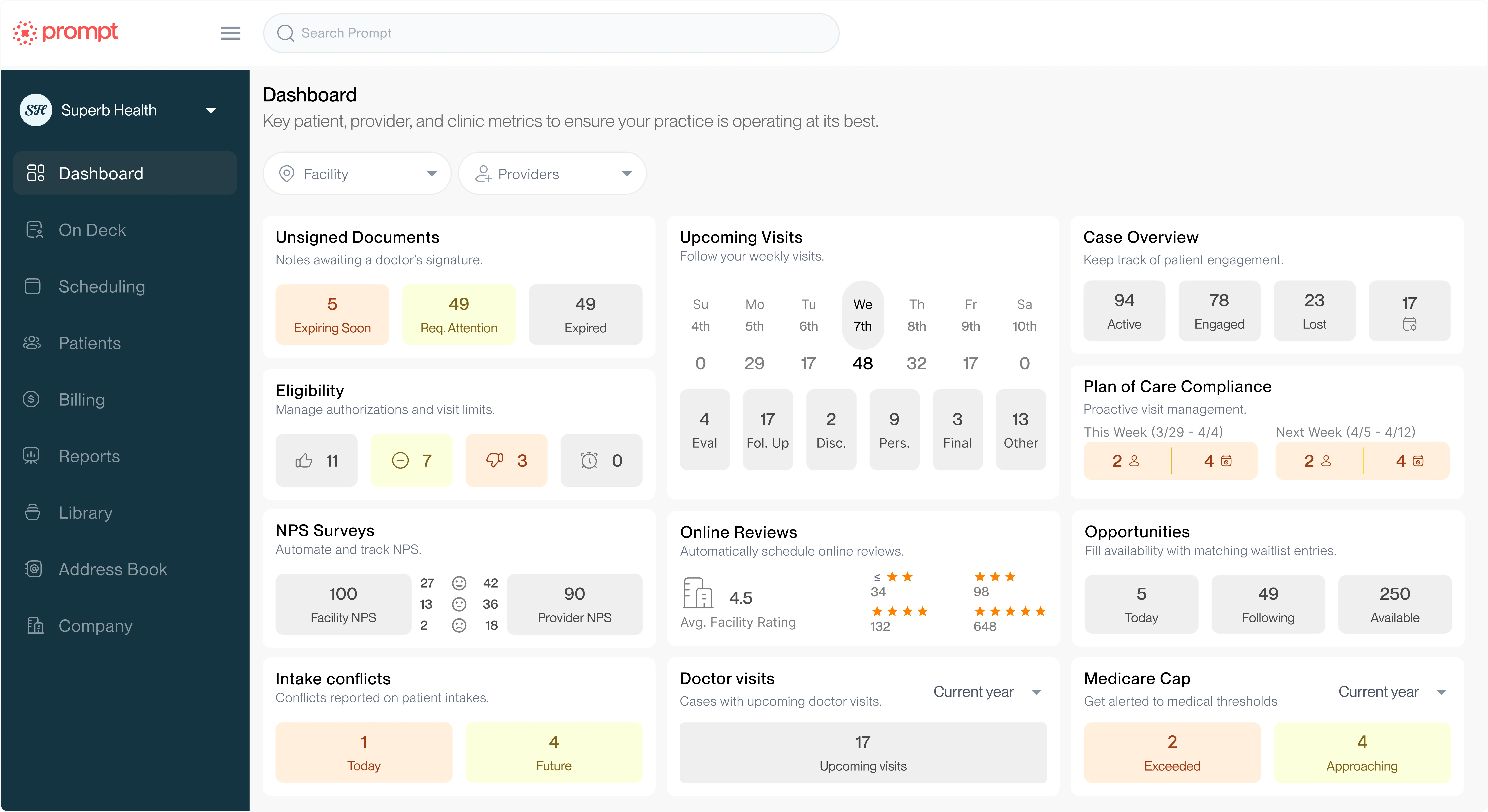
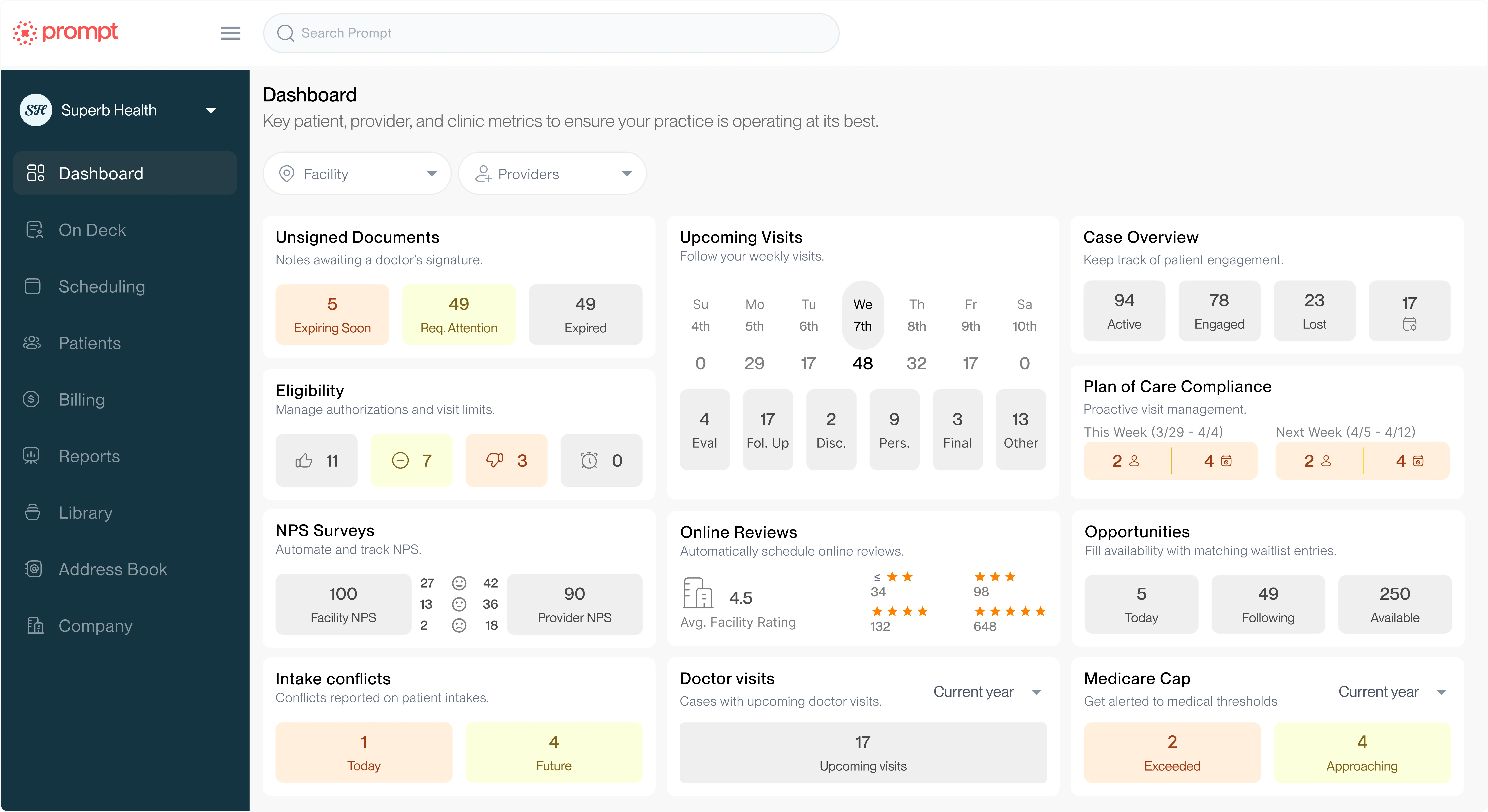
Help your practice grow
From intake to insights, Prompt is the all-in-one platform you need