See Prompt in action!
As a rehab professional, you’ve probably been supporting patients between appointments for years: checking on home exercise programs, answering questions, and adjusting plans when something isn’t working.
In other words, you’ve likely been providing remote therapeutic monitoring (RTM) without realizing it (or billing for it).
Head of Clinical Innovation at Prompt Marla Ranieri says “as providers, we all go the extra mile all the time. And that basically means we've been practicing remote therapeutic monitoring all along. We just weren't really reimbursed for it.”
In this article, we’ll clarify what RTM is, why it matters for modern practices, and how clinics use it to improve continuity of care and capture reimbursement for work they’re already doing.
RTM is a set of CPT codes that recognize clinically meaningful touch points happening outside the 4 walls of the clinic.
Vikram Sethuraman, founder of Engage (formerly PT Wired), explains it simply: “RTM refers to a set of CPT codes that allow providers to essentially now bill for monitoring patients and engaging with patients in between clinic visits. Basically, a lot of things that people have been doing for years.”
The earliest adopters of RTM were drawn by revenue diversification, but over time, the rationale broadened.
“ More recently, it's become even more of a hot topic because the data that we've seen in terms of how RTM impacts outcomes and how it impacts retention and plan of care length. So since it's been a couple years, there are a lot more insights that we have into what implementing RTM can do for a practice,” Vikram says.
The RTM code set includes 5 primary CPT codes:
In 2026, the Centers for Medicare & Medicaid Services (CMS) introduced 2 additional RTM codes:
You’re likely already doing all these tasks in the course of your normal clinic life. These codes allow you to formally bill for those activities and get paid for the work you’re already doing.
Think about a typical week in your clinic.
A patient messages to say an exercise is flaring their pain; your clinician tweaks the plan before the next appointment. Another patient needs encouragement to stay consistent with their HEP; someone on your team checks in.
All of these interactions are valuable for patient care, but without RTM they remain invisible to payers. RTM simply formalizes this ongoing communication and turns it into something reimbursable.
Rather than giving away hours of clinician time for free, practices that adopt RTM can get paid for the support they’re providing.
AIM Sports Medicine & Physical Therapy owner Carina Testa recognized this right away: “I thought, ‘Wow, this is something we actually are already doing. Why not actually get paid for this time?’”
Once her team aligned on consistent check-ins through Engage’s RTM app, “it just brought better engagement between patients and providers. And now we were actually getting paid for our expertise and our services, things that we were already doing,” she says.
There’s no one right way to implement RTM, Vikram says: “It all depends on the differences in the clinic.” Here are a few examples of the different ways clinics use RTM:
Rehab can easily devolve into disconnected weekly meetings. Bryan Lang, owner at Whole Body Health, describes it as “just a series of touch points. ‘See me this week, then see me next week.’ So having something like RTM allows for more of a continuum of care throughout that week with check-ins,” he says.
That added continuity helps patients stay accountable, surface problems sooner, and get timely tweaks to their HEP, all without waiting for the next in-person slot. Over time, Bryan’s data told a clear story: “Far and away people who are enrolled in RTM have more visits per plan of care at discharge and a longer length of stay,” he says.
Engage’s internal data tells the same story. RTM patients tend to complete 5.5 additional visits per POC than non-RTM patients, leading to more consistent care and better patient outcomes.
Patients respond better when they feel supported between visits. Carina saw this immediately.
“RTM brought in more engagement. Our providers were more consistent, and it got better engagement with our patients because now they were also accountable,” she says.
Beyond structure, RTM check-ins add an additional human connection, particularly for older adults or people who may be less comfortable with technology but want to learn.
“Some of our clients are widows or widowers, and they really enjoy our RTM app. It keeps them engaged on a very social level,” Bounce Back PT owner Charan Chadha says. “We try to create this almost like a gaming system. That's how we've gotten really good engagement… because the aging community also wants to be relevant.
They have grandkids that are all gaming, so we use this as a gaming system and they get these little congratulations at the end of the month and they love it. So for those of you that were asking questions about, how do you keep that going? We make it fun.”
And the results speak for themselves: Bounce Back’s arrival rate is nearly 97% after implementing RTM.
The numbers add up quickly. Even a modest RTM program can bring in thousands of dollars per year.
For example, if 50 patients in your clinic qualify for RTM, and each generates an average of $60-$100 in reimbursement per month, that’s $3,000-$5,000 in added revenue each month. Over the course of a year, your clinic could see $36,000-$60,000 in added revenue.
And this doesn’t require adding staff or increasing the number of in-person visits. It’s about capturing revenue from work that’s already happening in your clinic every day.
RTM isn’t only about increased clinic revenue. It can also transform the way patients experience their care.
When patients know their progress is being tracked between visits, they tend to feel more accountable to their home programs. Clinicians can spot issues more quickly and adjust exercises before they become bigger problems, rather than waiting until the next appointment.
This ongoing connection increases engagement and keeps patients from dropping off their plans prematurely. Patients also report feeling more supported when they know their therapist is following their progress and checking in.
RTM strengthens the relationship between patient and provider, leading to better outcomes and higher satisfaction.
For most outpatient rehab practices, the answer is yes. If your team prescribes home exercises, communicates with patients between visits, and makes adjustments based on reported progress, then you’re already doing the kind of work that RTM was built to capture.
The difference is that clinics using RTM can turn those efforts into reimbursement, while others are giving that time away for free.
Implementing RTM doesn’t require an overhaul of your workflow. The first step is to look at how your team already engages with patients outside of visits.
From there, adopting a simple system for tracking and documenting those interactions is usually all it takes to begin billing for them.
With proper clinician training and consistent documentation, your clinic can start capturing RTM revenue quickly.
RTM isn’t just a billing exercise. It’s a practical framework for acknowledging the clinical work that connects appointments and keeps patients moving forward. Bryan calls it “a win-win” for everybody: better continuity and accountability for patients, and fair reimbursement for clinics already doing the work.
If your team checks in, adjusts HEPs, and supports patients between visits, you’re practicing the spirit of RTM today. Formalizing that effort helps patients finish stronger and ensures your clinic is recognized for the care you deliver.
{{demo-cta-banner}}
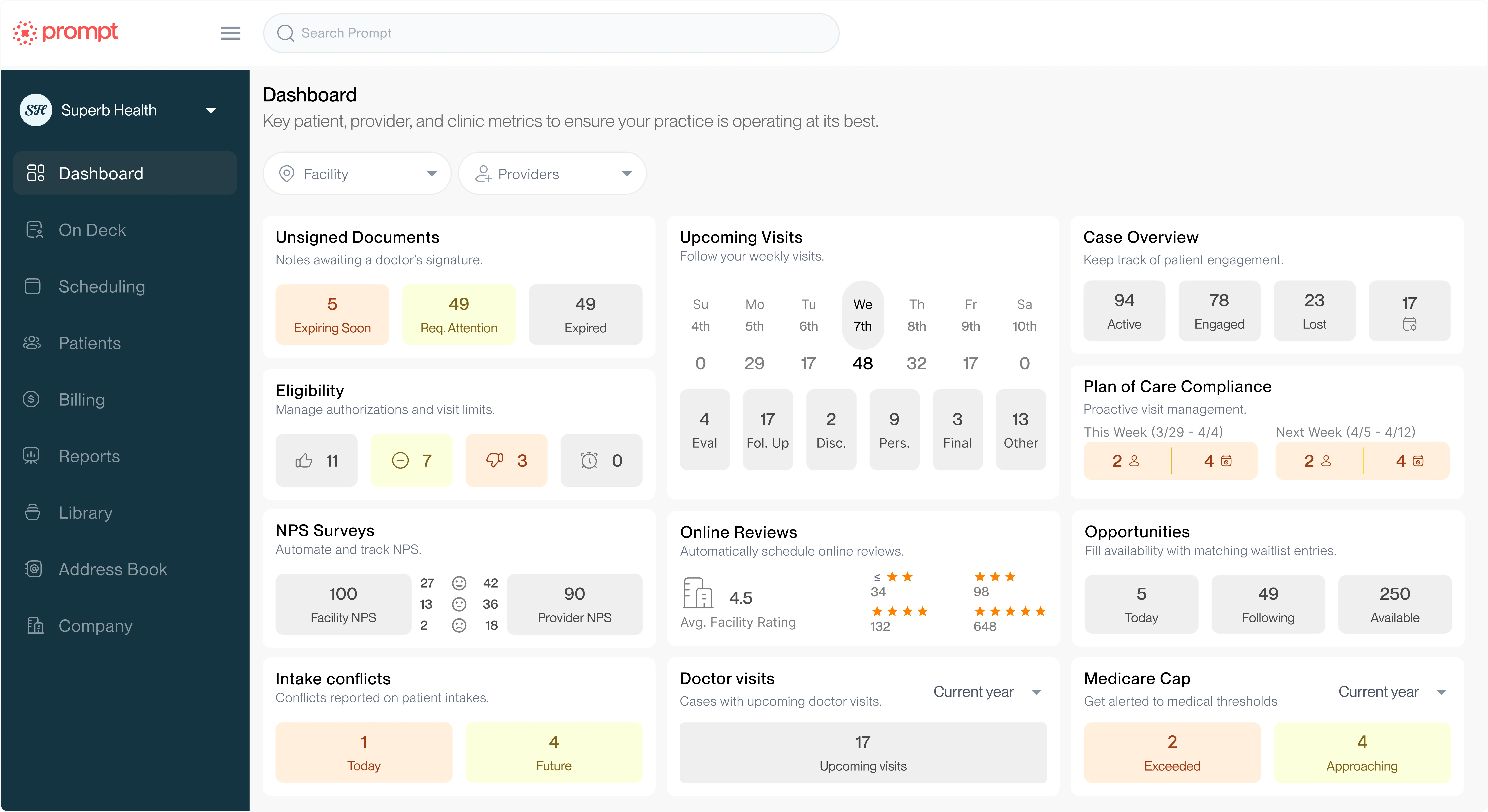
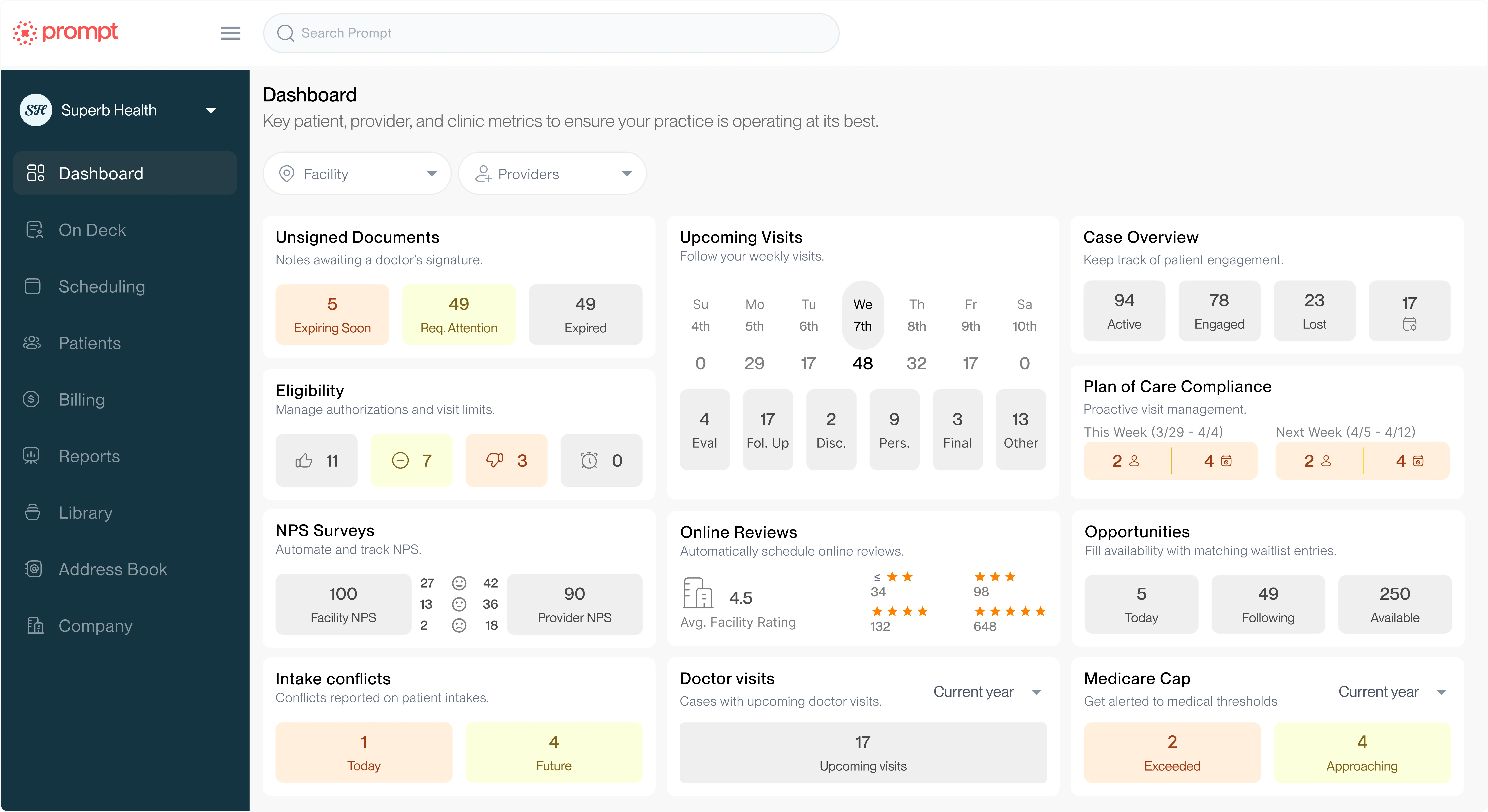
Help your practice grow
From intake to insights, Prompt is the all-in-one platform you need